Caspian Products
- Ampoules
- Anlagesics, Anti-inflammatory Drugs
- Antimyasthenics ,Muscle Relaxants
- Antiparkinson Drugs, Antidepressants,Antiepileptics, Anxiolytic Sedative, Hypnotics and Antipsychotics
- Hormonal Drugs
- Antihistamines, Bronchodilators
- Cardiovascular Drugs,Electrolytes
- Corticosteroids
- General Anaesthetics, Local Anaesthetics
- Antibacterials
- Gastrointestinal Drugs
- Nutritional Agents and Vitamins
- Antagonists
- Suppository
- Syrups & Oral Solutions
- Ointments, Creams & Gels
- Vial
- Prefilled Syringe
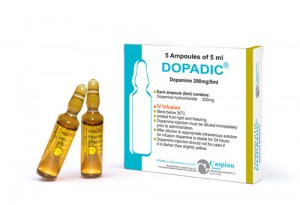
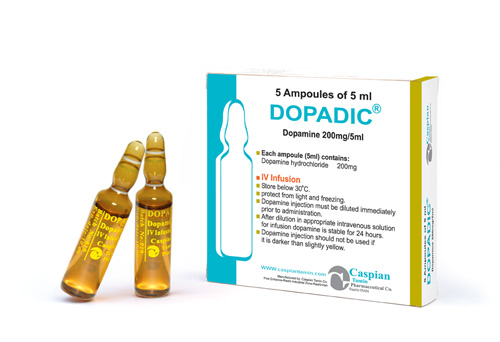
Dopamine
Pharmacology
Dopamine is a natural catecholamine formed by the decarboxylation of 3,4-dihydroxyphenylalanine (DOPA). It is a precursor to norepinephrine in noradrenergic nerves and is also a neurotransmitter in certain areas of the central nervous system, especially in the nigrostriatal tract, and in a few peripheral sympathetic nerves.
Dopamine produces positive chronotropic and inotropic effects on the myocardium, resulting in increased heart rate and cardiac contractility. This is accomplished directly by exerting an agonist action on beta-adrenoceptors and indirectly by causing release of norepinephrine from storage sites in sympathetic nerve endings.
Pharmacokinetics:
Dopamine (dopamine hydrochloride) 's onset of action occurs within five minutes of intravenous administration, and with dopamine (dopamine hydrochloride) 's plasma half-life of about two minutes, the duration of action is less than ten minutes. If monoamine oxidase (MAO) inhibitors are present, however, the duration may increase to one hour. The drug is widely distributed in the body but does not cross the blood-brain barrier to a significant extent. Dopamine (dopamine hydrochloride) is metabolized in the liver, kidney, and plasma by MAO and catechol-O-methyltransferase to the inactive compounds homovanillic acid (HVA) and 3,4-dihydroxyphenylacetic acid. About 25% of the dose is taken up into specialized neurosecretory vesicles (the adrenergic nerve terminals), where it is hydroxylated to form norepinephrine. It has been reported that about 80% of the drug is excreted in the urine within 24 hours, primarily as HVA and its sulfate and glucuronide conjugates and as 3,4-dihydroxyphenylacetic acid. A very small portion is excreted unchanged.
Indications:
Dopamine is indicated for the correction of hemodynamic imbalances present in the shock syndrome due to myocardial infarctions, trauma, endotoxic septicemia, open heart surgery, renal failure, and chronic cardiac decompensation as in congestive failure.
Administration and Dosage:
Dopamine should not be used in patients with pheochromocytoma.
Dopamine should not be administered in the presence of uncorrected tachyarrhythmias or ventricular fibrillation.
Precautions:
Careful monitoring required - Close monitoring of the following indices-urine flow, cardiac output and blood pressure - during Dopamine infusion is necessary as in the case of any adrenergic agent.
Avoid hypovolemia - Prior to treatment with Dopamine , hypovolemia should be fully corrected, if possible with either whole blood or plasma as indicated. Monitoring of central venous pressure of left ventricular filling pressure may be helpful in detecting and treating hypovolemia.
Hypoxia, Hypercapnia, Acidosis - These conditions which may also reduce the effectiveness and/or increase the incidence of adverse effects of dopamine, must be identified and corrected prior to, or concurrently with administration of dopamine.
Ventricular Arrhythmias - If an increased number of ectopic beats are observed, the dose should be reduced if possible.
Decreased Pulse Pressure - If a disproportionate rise in the diastolic pressure (i.e., a marked decrease in the pulse pressure) is observed in patients receiving Dopamine, the infusion rate should be decreased and the patient observed carefully for further evidence of predominant vasoconstrictor activity, unless such an effect is desired.
Hypotension - At lower infusion rates, if hypotension occurs, the infusion rate should be rapidly increased until adequate blood pressure is obtained. If hypotension persists, dopamine should be discontinued and a more potent vasoconstrictor agent such as norepinephrine should be administered.
Extravasation - Dopamine should be infused into a large vein whenever possible to prevent the possibility of extravasation into tissue adjacent to the infusion site. Extravasation may cause necrosis and sloughing of surrounding tissue. Large veins of the actecubital fossa are preferred to veins in the dorsum of the hand or ankle. Less suitable infusion sites should be used only if the patient's condition requires immediate attention. The physician should switch to more suitable sites as rapidly as possible. The infusion site should be continuously monitored for free flow.
Occlusive vascular disease - Patients with a history of occlusive vascular disease (for example, atheroscierosis, arterial embolism, and Raynaud's disease, cold injury, diabetic endarteritis, and Buergers disease) should be closely monitored for any changes in color or temperature of the skin in the extremities. If a change in skin color or temperature occurs and is thought to be the result of compromised circulation to the extremities, the benefits of continued Dopamine infusion should be weighed against the risk of possible necrosis. This condition may be reversed by either decreasing or discontinuing the rate of infusion.
Drug Interactions:
• droperidol ;
• epinephrine ;
• haloperidol ;
• midodrine ;
• phenytoin (dilantin);
• vasopressin ;
• a diuretic (water pill);
• an antidepressant such as amitriptyline , doxepin , nortriptyline , and others;
• a beta blocker such as atenolol , carvedilol , labetalol , metoprolol , nadolol , propranolol , sotalol , and others;
• cough or cold medicine that contains an antihistamine or decongestant;
• ergot medicine such as ergotamine , dihydroergotamine , ergonovine , or methylergonovine (Methergine);
• a phenothiazine such as chlorpromazine , fluphenazine , perphenazine , prochlorperazine , promethazine , thioridazine (Mellaril), or trifluoperazine ;
Side Effects:
• chest pain;
• fast, slow, or pounding heartbeats;
• painful or difficult urination, blood in your urine;
• weakness, confusion, swelling in your feet or ankles, urinating less than usual or not at all;
• weak or shallow breathing;
• feeling like you might pass out, even while lying down;
• burning, pain, or swelling around the IV needle;
• cold feeling, numbness, or blue-colored appearance in your hands or feet; or
• darkening or skin changes in your hands or feet.
Less serious dopamine side effects may include:
• headache;
• feeling anxious;
• nausea, vomiting; or
• chills, goosebumps.
Storage:
• Store below 30 C°
• Protect from light and freezing
Packing:
• Injection 200mg/5ml: Box of 5 ampoules
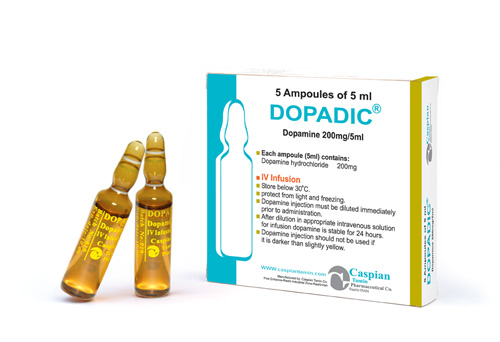
DOPADIC®
Injection 200mg/5ml
Cardiovascular Drugs
Inotropic Agents
Category C
Dopamine is a natural catecholamine formed by the decarboxylation of 3,4-dihydroxyphenylalanine (DOPA). It is a precursor to norepinephrine in noradrenergic nerves and is also a neurotransmitter in certain areas of the central nervous system, especially in the nigrostriatal tract, and in a few peripheral sympathetic nerves.
Dopamine produces positive chronotropic and inotropic effects on the myocardium, resulting in increased heart rate and cardiac contractility. This is accomplished directly by exerting an agonist action on beta-adrenoceptors and indirectly by causing release of norepinephrine from storage sites in sympathetic nerve endings.
Dopamine (dopamine hydrochloride) 's onset of action occurs within five minutes of intravenous administration, and with dopamine (dopamine hydrochloride) 's plasma half-life of about two minutes, the duration of action is less than ten minutes. If monoamine oxidase (MAO) inhibitors are present, however, the duration may increase to one hour. The drug is widely distributed in the body but does not cross the blood-brain barrier to a significant extent. Dopamine (dopamine hydrochloride) is metabolized in the liver, kidney, and plasma by MAO and catechol-O-methyltransferase to the inactive compounds homovanillic acid (HVA) and 3,4-dihydroxyphenylacetic acid. About 25% of the dose is taken up into specialized neurosecretory vesicles (the adrenergic nerve terminals), where it is hydroxylated to form norepinephrine. It has been reported that about 80% of the drug is excreted in the urine within 24 hours, primarily as HVA and its sulfate and glucuronide conjugates and as 3,4-dihydroxyphenylacetic acid. A very small portion is excreted unchanged.
Dopamine is indicated for the correction of hemodynamic imbalances present in the shock syndrome due to myocardial infarctions, trauma, endotoxic septicemia, open heart surgery, renal failure, and chronic cardiac decompensation as in congestive failure.
Dopamine should not be used in patients with pheochromocytoma.
Dopamine should not be administered in the presence of uncorrected tachyarrhythmias or ventricular fibrillation.
Careful monitoring required - Close monitoring of the following indices-urine flow, cardiac output and blood pressure - during Dopamine infusion is necessary as in the case of any adrenergic agent.
Avoid hypovolemia - Prior to treatment with Dopamine , hypovolemia should be fully corrected, if possible with either whole blood or plasma as indicated. Monitoring of central venous pressure of left ventricular filling pressure may be helpful in detecting and treating hypovolemia.
Hypoxia, Hypercapnia, Acidosis - These conditions which may also reduce the effectiveness and/or increase the incidence of adverse effects of dopamine, must be identified and corrected prior to, or concurrently with administration of dopamine.
Ventricular Arrhythmias - If an increased number of ectopic beats are observed, the dose should be reduced if possible.
Decreased Pulse Pressure - If a disproportionate rise in the diastolic pressure (i.e., a marked decrease in the pulse pressure) is observed in patients receiving Dopamine, the infusion rate should be decreased and the patient observed carefully for further evidence of predominant vasoconstrictor activity, unless such an effect is desired.
Hypotension - At lower infusion rates, if hypotension occurs, the infusion rate should be rapidly increased until adequate blood pressure is obtained. If hypotension persists, dopamine should be discontinued and a more potent vasoconstrictor agent such as norepinephrine should be administered.
Extravasation - Dopamine should be infused into a large vein whenever possible to prevent the possibility of extravasation into tissue adjacent to the infusion site. Extravasation may cause necrosis and sloughing of surrounding tissue. Large veins of the actecubital fossa are preferred to veins in the dorsum of the hand or ankle. Less suitable infusion sites should be used only if the patient's condition requires immediate attention. The physician should switch to more suitable sites as rapidly as possible. The infusion site should be continuously monitored for free flow.
Occlusive vascular disease - Patients with a history of occlusive vascular disease (for example, atheroscierosis, arterial embolism, and Raynaud's disease, cold injury, diabetic endarteritis, and Buergers disease) should be closely monitored for any changes in color or temperature of the skin in the extremities. If a change in skin color or temperature occurs and is thought to be the result of compromised circulation to the extremities, the benefits of continued Dopamine infusion should be weighed against the risk of possible necrosis. This condition may be reversed by either decreasing or discontinuing the rate of infusion.
• droperidol ;
• epinephrine ;
• haloperidol ;
• midodrine ;
• phenytoin (dilantin);
• vasopressin ;
• a diuretic (water pill);
• an antidepressant such as amitriptyline , doxepin , nortriptyline , and others;
• a beta blocker such as atenolol , carvedilol , labetalol , metoprolol , nadolol , propranolol , sotalol , and others;
• cough or cold medicine that contains an antihistamine or decongestant;
• ergot medicine such as ergotamine , dihydroergotamine , ergonovine , or methylergonovine (Methergine);
• a phenothiazine such as chlorpromazine , fluphenazine , perphenazine , prochlorperazine , promethazine , thioridazine (Mellaril), or trifluoperazine ;
• chest pain;
• fast, slow, or pounding heartbeats;
• painful or difficult urination, blood in your urine;
• weakness, confusion, swelling in your feet or ankles, urinating less than usual or not at all;
• weak or shallow breathing;
• feeling like you might pass out, even while lying down;
• burning, pain, or swelling around the IV needle;
• cold feeling, numbness, or blue-colored appearance in your hands or feet; or
• darkening or skin changes in your hands or feet.
Less serious dopamine side effects may include:
• headache;
• feeling anxious;
• nausea, vomiting; or
• chills, goosebumps.
• Store below 30 C°
• Protect from light and freezing
• Injection 200mg/5ml: Box of 5 ampoules
 )
)
[field_administration_and_dosage] => Array
(
[0] => Array
(
[value] => Dopamine should not be used in patients with pheochromocytoma.
Dopamine should not be administered in the presence of uncorrected tachyarrhythmias or ventricular fibrillation.
[format] => 1
[safe] =>
)
)
[field_administration_and_dosage] => Array
(
[0] => Array
(
[value] => Dopamine should not be used in patients with pheochromocytoma.
Dopamine should not be administered in the presence of uncorrected tachyarrhythmias or ventricular fibrillation.
[format] => 1
[safe] => Dopamine should not be used in patients with pheochromocytoma.
Dopamine should not be administered in the presence of uncorrected tachyarrhythmias or ventricular fibrillation.
Dopamine should not be used in patients with pheochromocytoma.
Dopamine should not be administered in the presence of uncorrected tachyarrhythmias or ventricular fibrillation.
DOPADIC®
[view] =>DOPADIC®
) ) [field_contraindications] => Array ( [0] => Array ( [value] => [format] => [safe] => [view] => ) ) [field_dosage_form] => Array ( [0] => Array ( [value] => Injection 200mg/5ml [format] => 1 [safe] =>Injection 200mg/5ml
[view] =>Injection 200mg/5ml
) ) [field_drug_interactions] => Array ( [0] => Array ( [value] => • droperidol ; • epinephrine ; • haloperidol ; • midodrine ; • phenytoin (dilantin); • vasopressin ; • a diuretic (water pill); • an antidepressant such as amitriptyline , doxepin , nortriptyline , and others; • a beta blocker such as atenolol , carvedilol , labetalol , metoprolol , nadolol , propranolol , sotalol , and others; • cough or cold medicine that contains an antihistamine or decongestant; • ergot medicine such as ergotamine , dihydroergotamine , ergonovine , or methylergonovine (Methergine); • a phenothiazine such as chlorpromazine , fluphenazine , perphenazine , prochlorperazine , promethazine , thioridazine (Mellaril), or trifluoperazine ; [format] => 1 [safe] =>• droperidol ;
• epinephrine ;
• haloperidol ;
• midodrine ;
• phenytoin (dilantin);
• vasopressin ;
• a diuretic (water pill);
• an antidepressant such as amitriptyline , doxepin , nortriptyline , and others;
• a beta blocker such as atenolol , carvedilol , labetalol , metoprolol , nadolol , propranolol , sotalol , and others;
• cough or cold medicine that contains an antihistamine or decongestant;
• ergot medicine such as ergotamine , dihydroergotamine , ergonovine , or methylergonovine (Methergine);
• a phenothiazine such as chlorpromazine , fluphenazine , perphenazine , prochlorperazine , promethazine , thioridazine (Mellaril), or trifluoperazine ;
• droperidol ;
• epinephrine ;
• haloperidol ;
• midodrine ;
• phenytoin (dilantin);
• vasopressin ;
• a diuretic (water pill);
• an antidepressant such as amitriptyline , doxepin , nortriptyline , and others;
• a beta blocker such as atenolol , carvedilol , labetalol , metoprolol , nadolol , propranolol , sotalol , and others;
• cough or cold medicine that contains an antihistamine or decongestant;
• ergot medicine such as ergotamine , dihydroergotamine , ergonovine , or methylergonovine (Methergine);
• a phenothiazine such as chlorpromazine , fluphenazine , perphenazine , prochlorperazine , promethazine , thioridazine (Mellaril), or trifluoperazine ;
Dopamine is indicated for the correction of hemodynamic imbalances present in the shock syndrome due to myocardial infarctions, trauma, endotoxic septicemia, open heart surgery, renal failure, and chronic cardiac decompensation as in congestive failure.
[view] =>Dopamine is indicated for the correction of hemodynamic imbalances present in the shock syndrome due to myocardial infarctions, trauma, endotoxic septicemia, open heart surgery, renal failure, and chronic cardiac decompensation as in congestive failure.
) ) [field_packing] => Array ( [0] => Array ( [value] => • Injection 200mg/5ml: Box of 5 ampoules [format] => 1 [safe] =>• Injection 200mg/5ml: Box of 5 ampoules
[view] =>• Injection 200mg/5ml: Box of 5 ampoules
) ) [field_pdf] => Array ( [0] => Array ( [fid] => 195 [uid] => 1 [filename] => dopamine.pdf [filepath] => sites/default/files/pdf/dopamine.pdf [filemime] => application/pdf [filesize] => 155786 [status] => 1 [timestamp] => 1329491719 [list] => 1 [data] => [i18nsync] => 1 [nid] => 238 [view] => ) ) [field_pharmacokinetics] => Array ( [0] => Array ( [value] => Dopamine (dopamine hydrochloride) 's onset of action occurs within five minutes of intravenous administration, and with dopamine (dopamine hydrochloride) 's plasma half-life of about two minutes, the duration of action is less than ten minutes. If monoamine oxidase (MAO) inhibitors are present, however, the duration may increase to one hour. The drug is widely distributed in the body but does not cross the blood-brain barrier to a significant extent. Dopamine (dopamine hydrochloride) is metabolized in the liver, kidney, and plasma by MAO and catechol-O-methyltransferase to the inactive compounds homovanillic acid (HVA) and 3,4-dihydroxyphenylacetic acid. About 25% of the dose is taken up into specialized neurosecretory vesicles (the adrenergic nerve terminals), where it is hydroxylated to form norepinephrine. It has been reported that about 80% of the drug is excreted in the urine within 24 hours, primarily as HVA and its sulfate and glucuronide conjugates and as 3,4-dihydroxyphenylacetic acid. A very small portion is excreted unchanged. [format] => 1 [safe] =>Dopamine (dopamine hydrochloride) 's onset of action occurs within five minutes of intravenous administration, and with dopamine (dopamine hydrochloride) 's plasma half-life of about two minutes, the duration of action is less than ten minutes. If monoamine oxidase (MAO) inhibitors are present, however, the duration may increase to one hour. The drug is widely distributed in the body but does not cross the blood-brain barrier to a significant extent. Dopamine (dopamine hydrochloride) is metabolized in the liver, kidney, and plasma by MAO and catechol-O-methyltransferase to the inactive compounds homovanillic acid (HVA) and 3,4-dihydroxyphenylacetic acid. About 25% of the dose is taken up into specialized neurosecretory vesicles (the adrenergic nerve terminals), where it is hydroxylated to form norepinephrine. It has been reported that about 80% of the drug is excreted in the urine within 24 hours, primarily as HVA and its sulfate and glucuronide conjugates and as 3,4-dihydroxyphenylacetic acid. A very small portion is excreted unchanged.
[view] =>Dopamine (dopamine hydrochloride) 's onset of action occurs within five minutes of intravenous administration, and with dopamine (dopamine hydrochloride) 's plasma half-life of about two minutes, the duration of action is less than ten minutes. If monoamine oxidase (MAO) inhibitors are present, however, the duration may increase to one hour. The drug is widely distributed in the body but does not cross the blood-brain barrier to a significant extent. Dopamine (dopamine hydrochloride) is metabolized in the liver, kidney, and plasma by MAO and catechol-O-methyltransferase to the inactive compounds homovanillic acid (HVA) and 3,4-dihydroxyphenylacetic acid. About 25% of the dose is taken up into specialized neurosecretory vesicles (the adrenergic nerve terminals), where it is hydroxylated to form norepinephrine. It has been reported that about 80% of the drug is excreted in the urine within 24 hours, primarily as HVA and its sulfate and glucuronide conjugates and as 3,4-dihydroxyphenylacetic acid. A very small portion is excreted unchanged.
) ) [field_pharmacological_category] => Array ( [0] => Array ( [value] => Cardiovascular Drugs [format] => 1 [safe] =>Cardiovascular Drugs
[view] =>Cardiovascular Drugs
) ) [field_precautions] => Array ( [0] => Array ( [value] =>Careful monitoring required - Close monitoring of the following indices-urine flow, cardiac output and blood pressure - during Dopamine infusion is necessary as in the case of any adrenergic agent.
Avoid hypovolemia - Prior to treatment with Dopamine , hypovolemia should be fully corrected, if possible with either whole blood or plasma as indicated. Monitoring of central venous pressure of left ventricular filling pressure may be helpful in detecting and treating hypovolemia.
Hypoxia, Hypercapnia, Acidosis - These conditions which may also reduce the effectiveness and/or increase the incidence of adverse effects of dopamine, must be identified and corrected prior to, or concurrently with administration of dopamine.
Ventricular Arrhythmias - If an increased number of ectopic beats are observed, the dose should be reduced if possible.
Decreased Pulse Pressure - If a disproportionate rise in the diastolic pressure (i.e., a marked decrease in the pulse pressure) is observed in patients receiving Dopamine, the infusion rate should be decreased and the patient observed carefully for further evidence of predominant vasoconstrictor activity, unless such an effect is desired.
Hypotension - At lower infusion rates, if hypotension occurs, the infusion rate should be rapidly increased until adequate blood pressure is obtained. If hypotension persists, dopamine should be discontinued and a more potent vasoconstrictor agent such as norepinephrine should be administered.
Extravasation - Dopamine should be infused into a large vein whenever possible to prevent the possibility of extravasation into tissue adjacent to the infusion site. Extravasation may cause necrosis and sloughing of surrounding tissue. Large veins of the actecubital fossa are preferred to veins in the dorsum of the hand or ankle. Less suitable infusion sites should be used only if the patient's condition requires immediate attention. The physician should switch to more suitable sites as rapidly as possible. The infusion site should be continuously monitored for free flow.
Occlusive vascular disease - Patients with a history of occlusive vascular disease (for example, atheroscierosis, arterial embolism, and Raynaud's disease, cold injury, diabetic endarteritis, and Buergers disease) should be closely monitored for any changes in color or temperature of the skin in the extremities. If a change in skin color or temperature occurs and is thought to be the result of compromised circulation to the extremities, the benefits of continued Dopamine infusion should be weighed against the risk of possible necrosis. This condition may be reversed by either decreasing or discontinuing the rate of infusion.
Careful monitoring required - Close monitoring of the following indices-urine flow, cardiac output and blood pressure - during Dopamine infusion is necessary as in the case of any adrenergic agent.
Avoid hypovolemia - Prior to treatment with Dopamine , hypovolemia should be fully corrected, if possible with either whole blood or plasma as indicated. Monitoring of central venous pressure of left ventricular filling pressure may be helpful in detecting and treating hypovolemia.
Hypoxia, Hypercapnia, Acidosis - These conditions which may also reduce the effectiveness and/or increase the incidence of adverse effects of dopamine, must be identified and corrected prior to, or concurrently with administration of dopamine.
Ventricular Arrhythmias - If an increased number of ectopic beats are observed, the dose should be reduced if possible.
Decreased Pulse Pressure - If a disproportionate rise in the diastolic pressure (i.e., a marked decrease in the pulse pressure) is observed in patients receiving Dopamine, the infusion rate should be decreased and the patient observed carefully for further evidence of predominant vasoconstrictor activity, unless such an effect is desired.
Hypotension - At lower infusion rates, if hypotension occurs, the infusion rate should be rapidly increased until adequate blood pressure is obtained. If hypotension persists, dopamine should be discontinued and a more potent vasoconstrictor agent such as norepinephrine should be administered.
Extravasation - Dopamine should be infused into a large vein whenever possible to prevent the possibility of extravasation into tissue adjacent to the infusion site. Extravasation may cause necrosis and sloughing of surrounding tissue. Large veins of the actecubital fossa are preferred to veins in the dorsum of the hand or ankle. Less suitable infusion sites should be used only if the patient's condition requires immediate attention. The physician should switch to more suitable sites as rapidly as possible. The infusion site should be continuously monitored for free flow.
Occlusive vascular disease - Patients with a history of occlusive vascular disease (for example, atheroscierosis, arterial embolism, and Raynaud's disease, cold injury, diabetic endarteritis, and Buergers disease) should be closely monitored for any changes in color or temperature of the skin in the extremities. If a change in skin color or temperature occurs and is thought to be the result of compromised circulation to the extremities, the benefits of continued Dopamine infusion should be weighed against the risk of possible necrosis. This condition may be reversed by either decreasing or discontinuing the rate of infusion.
Careful monitoring required - Close monitoring of the following indices-urine flow, cardiac output and blood pressure - during Dopamine infusion is necessary as in the case of any adrenergic agent.
Avoid hypovolemia - Prior to treatment with Dopamine , hypovolemia should be fully corrected, if possible with either whole blood or plasma as indicated. Monitoring of central venous pressure of left ventricular filling pressure may be helpful in detecting and treating hypovolemia.
Hypoxia, Hypercapnia, Acidosis - These conditions which may also reduce the effectiveness and/or increase the incidence of adverse effects of dopamine, must be identified and corrected prior to, or concurrently with administration of dopamine.
Ventricular Arrhythmias - If an increased number of ectopic beats are observed, the dose should be reduced if possible.
Decreased Pulse Pressure - If a disproportionate rise in the diastolic pressure (i.e., a marked decrease in the pulse pressure) is observed in patients receiving Dopamine, the infusion rate should be decreased and the patient observed carefully for further evidence of predominant vasoconstrictor activity, unless such an effect is desired.
Hypotension - At lower infusion rates, if hypotension occurs, the infusion rate should be rapidly increased until adequate blood pressure is obtained. If hypotension persists, dopamine should be discontinued and a more potent vasoconstrictor agent such as norepinephrine should be administered.
Extravasation - Dopamine should be infused into a large vein whenever possible to prevent the possibility of extravasation into tissue adjacent to the infusion site. Extravasation may cause necrosis and sloughing of surrounding tissue. Large veins of the actecubital fossa are preferred to veins in the dorsum of the hand or ankle. Less suitable infusion sites should be used only if the patient's condition requires immediate attention. The physician should switch to more suitable sites as rapidly as possible. The infusion site should be continuously monitored for free flow.
Occlusive vascular disease - Patients with a history of occlusive vascular disease (for example, atheroscierosis, arterial embolism, and Raynaud's disease, cold injury, diabetic endarteritis, and Buergers disease) should be closely monitored for any changes in color or temperature of the skin in the extremities. If a change in skin color or temperature occurs and is thought to be the result of compromised circulation to the extremities, the benefits of continued Dopamine infusion should be weighed against the risk of possible necrosis. This condition may be reversed by either decreasing or discontinuing the rate of infusion.
Category C
[view] =>Category C
) ) [field_references] => Array ( [0] => Array ( [value] => [format] => [safe] => [view] => ) ) [field_side_effects] => Array ( [0] => Array ( [value] => • chest pain; • fast, slow, or pounding heartbeats; • painful or difficult urination, blood in your urine; • weakness, confusion, swelling in your feet or ankles, urinating less than usual or not at all; • weak or shallow breathing; • feeling like you might pass out, even while lying down; • burning, pain, or swelling around the IV needle; • cold feeling, numbness, or blue-colored appearance in your hands or feet; or • darkening or skin changes in your hands or feet. Less serious dopamine side effects may include: • headache; • feeling anxious; • nausea, vomiting; or • chills, goosebumps. [format] => 1 [safe] =>• chest pain;
• fast, slow, or pounding heartbeats;
• painful or difficult urination, blood in your urine;
• weakness, confusion, swelling in your feet or ankles, urinating less than usual or not at all;
• weak or shallow breathing;
• feeling like you might pass out, even while lying down;
• burning, pain, or swelling around the IV needle;
• cold feeling, numbness, or blue-colored appearance in your hands or feet; or
• darkening or skin changes in your hands or feet.
Less serious dopamine side effects may include:
• headache;
• feeling anxious;
• nausea, vomiting; or
• chills, goosebumps.
• chest pain;
• fast, slow, or pounding heartbeats;
• painful or difficult urination, blood in your urine;
• weakness, confusion, swelling in your feet or ankles, urinating less than usual or not at all;
• weak or shallow breathing;
• feeling like you might pass out, even while lying down;
• burning, pain, or swelling around the IV needle;
• cold feeling, numbness, or blue-colored appearance in your hands or feet; or
• darkening or skin changes in your hands or feet.
Less serious dopamine side effects may include:
• headache;
• feeling anxious;
• nausea, vomiting; or
• chills, goosebumps.
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
Inotropic Agents
[view] =>Inotropic Agents
) ) [field_related_products] => Array ( [0] => Array ( [nid] => [i18nsync] => 1 [safe] => Array ( ) [view] => ) [1] => Array ( [nid] => [i18nsync] => 1 [safe] => Array ( ) [view] => ) [2] => Array ( [nid] => [i18nsync] => 1 [safe] => Array ( ) [view] => ) ) [taxonomy] => Array ( [7] => stdClass Object ( [tid] => 7 [vid] => 1 [name] => Cardiovascular Drugs,Electrolytes [description] => [weight] => 5 [language] => [trid] => 0 [v_weight_unused] => 0 ) ) [build_mode] => 0 [readmore] => 1 [content] => Array ( [field_one_image] => Array ( [#type_name] => product [#context] => full [#field_name] => field_one_image [#post_render] => Array ( [0] => content_field_wrapper_post_render ) [#weight] => -3 [field] => Array ( [#description] => [items] => Array ( [0] => Array ( [#formatter] => image_plain [#node] => stdClass Object *RECURSION* [#type_name] => product [#field_name] => field_one_image [#weight] => 0 [#theme] => imagefield_formatter_image_plain [#item] => Array ( [fid] => 194 [uid] => 1 [filename] => dopamine_s.jpg [filepath] => sites/default/files/images/dopamine_s.jpg [filemime] => image/jpeg [filesize] => 64100 [status] => 1 [timestamp] => 1329491444 [list] => 1 [data] => Array ( [alt] => [title] => ) [i18nsync] => 1 [nid] => 238 [#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] => )
[#title] =>
[#description] =>
[#children] =>
)
[#title] =>
[#description] =>
[#children] =>  [#printed] => 1
)
[#single] => 1
[#attributes] => Array
(
)
[#required] =>
[#parents] => Array
(
)
[#tree] =>
[#context] => full
[#page] => 1
[#field_name] => field_one_image
[#title] => Image
[#access] => 1
[#label_display] => above
[#teaser] =>
[#node] => stdClass Object
*RECURSION*
[#type] => content_field
[#children] =>
[#printed] => 1
)
[#single] => 1
[#attributes] => Array
(
)
[#required] =>
[#parents] => Array
(
)
[#tree] =>
[#context] => full
[#page] => 1
[#field_name] => field_one_image
[#title] => Image
[#access] => 1
[#label_display] => above
[#teaser] =>
[#node] => stdClass Object
*RECURSION*
[#type] => content_field
[#children] =>  [#printed] => 1
)
[#title] =>
[#description] =>
[#children] =>
[#printed] => 1
)
[#title] =>
[#description] =>
[#children] => 
DOPADIC®
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>DOPADIC®
) [#title] => [#description] => [#children] =>DOPADIC®
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_brand_name [#title] => Brand Name [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>DOPADIC®
[#printed] => 1 ) [#title] => [#description] => [#children] =>DOPADIC®
Injection 200mg/5ml
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Injection 200mg/5ml
) [#title] => [#description] => [#children] =>Injection 200mg/5ml
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_dosage_form [#title] => Dosage Form [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Injection 200mg/5ml
[#printed] => 1 ) [#title] => [#description] => [#children] =>Injection 200mg/5ml
Cardiovascular Drugs
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Cardiovascular Drugs
) [#title] => [#description] => [#children] =>Cardiovascular Drugs
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_pharmacological_category [#title] => Pharmacological Category [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Cardiovascular Drugs
[#printed] => 1 ) [#title] => [#description] => [#children] =>Cardiovascular Drugs
Inotropic Agents
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Inotropic Agents
) [#title] => [#description] => [#children] =>Inotropic Agents
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_therapeutic_category [#title] => Therapeutic Category [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Inotropic Agents
[#printed] => 1 ) [#title] => [#description] => [#children] =>Inotropic Agents
Category C
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Category C
) [#title] => [#description] => [#children] =>Category C
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_pregnancy_category [#title] => Pregnancy Category [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Category C
[#printed] => 1 ) [#title] => [#description] => [#children] =>Category C
Dopamine is a natural catecholamine formed by the decarboxylation of 3,4-dihydroxyphenylalanine (DOPA). It is a precursor to norepinephrine in noradrenergic nerves and is also a neurotransmitter in certain areas of the central nervous system, especially in the nigrostriatal tract, and in a few peripheral sympathetic nerves.
Dopamine produces positive chronotropic and inotropic effects on the myocardium, resulting in increased heart rate and cardiac contractility. This is accomplished directly by exerting an agonist action on beta-adrenoceptors and indirectly by causing release of norepinephrine from storage sites in sympathetic nerve endings.
Dopamine (dopamine hydrochloride) 's onset of action occurs within five minutes of intravenous administration, and with dopamine (dopamine hydrochloride) 's plasma half-life of about two minutes, the duration of action is less than ten minutes. If monoamine oxidase (MAO) inhibitors are present, however, the duration may increase to one hour. The drug is widely distributed in the body but does not cross the blood-brain barrier to a significant extent. Dopamine (dopamine hydrochloride) is metabolized in the liver, kidney, and plasma by MAO and catechol-O-methyltransferase to the inactive compounds homovanillic acid (HVA) and 3,4-dihydroxyphenylacetic acid. About 25% of the dose is taken up into specialized neurosecretory vesicles (the adrenergic nerve terminals), where it is hydroxylated to form norepinephrine. It has been reported that about 80% of the drug is excreted in the urine within 24 hours, primarily as HVA and its sulfate and glucuronide conjugates and as 3,4-dihydroxyphenylacetic acid. A very small portion is excreted unchanged.
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Dopamine (dopamine hydrochloride) 's onset of action occurs within five minutes of intravenous administration, and with dopamine (dopamine hydrochloride) 's plasma half-life of about two minutes, the duration of action is less than ten minutes. If monoamine oxidase (MAO) inhibitors are present, however, the duration may increase to one hour. The drug is widely distributed in the body but does not cross the blood-brain barrier to a significant extent. Dopamine (dopamine hydrochloride) is metabolized in the liver, kidney, and plasma by MAO and catechol-O-methyltransferase to the inactive compounds homovanillic acid (HVA) and 3,4-dihydroxyphenylacetic acid. About 25% of the dose is taken up into specialized neurosecretory vesicles (the adrenergic nerve terminals), where it is hydroxylated to form norepinephrine. It has been reported that about 80% of the drug is excreted in the urine within 24 hours, primarily as HVA and its sulfate and glucuronide conjugates and as 3,4-dihydroxyphenylacetic acid. A very small portion is excreted unchanged.
) [#title] => [#description] => [#children] =>Dopamine (dopamine hydrochloride) 's onset of action occurs within five minutes of intravenous administration, and with dopamine (dopamine hydrochloride) 's plasma half-life of about two minutes, the duration of action is less than ten minutes. If monoamine oxidase (MAO) inhibitors are present, however, the duration may increase to one hour. The drug is widely distributed in the body but does not cross the blood-brain barrier to a significant extent. Dopamine (dopamine hydrochloride) is metabolized in the liver, kidney, and plasma by MAO and catechol-O-methyltransferase to the inactive compounds homovanillic acid (HVA) and 3,4-dihydroxyphenylacetic acid. About 25% of the dose is taken up into specialized neurosecretory vesicles (the adrenergic nerve terminals), where it is hydroxylated to form norepinephrine. It has been reported that about 80% of the drug is excreted in the urine within 24 hours, primarily as HVA and its sulfate and glucuronide conjugates and as 3,4-dihydroxyphenylacetic acid. A very small portion is excreted unchanged.
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_pharmacokinetics [#title] => Pharmacokinetics [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Dopamine (dopamine hydrochloride) 's onset of action occurs within five minutes of intravenous administration, and with dopamine (dopamine hydrochloride) 's plasma half-life of about two minutes, the duration of action is less than ten minutes. If monoamine oxidase (MAO) inhibitors are present, however, the duration may increase to one hour. The drug is widely distributed in the body but does not cross the blood-brain barrier to a significant extent. Dopamine (dopamine hydrochloride) is metabolized in the liver, kidney, and plasma by MAO and catechol-O-methyltransferase to the inactive compounds homovanillic acid (HVA) and 3,4-dihydroxyphenylacetic acid. About 25% of the dose is taken up into specialized neurosecretory vesicles (the adrenergic nerve terminals), where it is hydroxylated to form norepinephrine. It has been reported that about 80% of the drug is excreted in the urine within 24 hours, primarily as HVA and its sulfate and glucuronide conjugates and as 3,4-dihydroxyphenylacetic acid. A very small portion is excreted unchanged.
[#printed] => 1 ) [#title] => [#description] => [#children] =>Dopamine (dopamine hydrochloride) 's onset of action occurs within five minutes of intravenous administration, and with dopamine (dopamine hydrochloride) 's plasma half-life of about two minutes, the duration of action is less than ten minutes. If monoamine oxidase (MAO) inhibitors are present, however, the duration may increase to one hour. The drug is widely distributed in the body but does not cross the blood-brain barrier to a significant extent. Dopamine (dopamine hydrochloride) is metabolized in the liver, kidney, and plasma by MAO and catechol-O-methyltransferase to the inactive compounds homovanillic acid (HVA) and 3,4-dihydroxyphenylacetic acid. About 25% of the dose is taken up into specialized neurosecretory vesicles (the adrenergic nerve terminals), where it is hydroxylated to form norepinephrine. It has been reported that about 80% of the drug is excreted in the urine within 24 hours, primarily as HVA and its sulfate and glucuronide conjugates and as 3,4-dihydroxyphenylacetic acid. A very small portion is excreted unchanged.
Dopamine is indicated for the correction of hemodynamic imbalances present in the shock syndrome due to myocardial infarctions, trauma, endotoxic septicemia, open heart surgery, renal failure, and chronic cardiac decompensation as in congestive failure.
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Dopamine is indicated for the correction of hemodynamic imbalances present in the shock syndrome due to myocardial infarctions, trauma, endotoxic septicemia, open heart surgery, renal failure, and chronic cardiac decompensation as in congestive failure.
) [#title] => [#description] => [#children] =>Dopamine is indicated for the correction of hemodynamic imbalances present in the shock syndrome due to myocardial infarctions, trauma, endotoxic septicemia, open heart surgery, renal failure, and chronic cardiac decompensation as in congestive failure.
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_indications [#title] => Indications [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Dopamine is indicated for the correction of hemodynamic imbalances present in the shock syndrome due to myocardial infarctions, trauma, endotoxic septicemia, open heart surgery, renal failure, and chronic cardiac decompensation as in congestive failure.
[#printed] => 1 ) [#title] => [#description] => [#children] =>Dopamine is indicated for the correction of hemodynamic imbalances present in the shock syndrome due to myocardial infarctions, trauma, endotoxic septicemia, open heart surgery, renal failure, and chronic cardiac decompensation as in congestive failure.
Dopamine should not be used in patients with pheochromocytoma.
Dopamine should not be administered in the presence of uncorrected tachyarrhythmias or ventricular fibrillation.
Dopamine should not be used in patients with pheochromocytoma.
Dopamine should not be administered in the presence of uncorrected tachyarrhythmias or ventricular fibrillation.
Dopamine should not be used in patients with pheochromocytoma.
Dopamine should not be administered in the presence of uncorrected tachyarrhythmias or ventricular fibrillation.
Dopamine should not be used in patients with pheochromocytoma.
Dopamine should not be administered in the presence of uncorrected tachyarrhythmias or ventricular fibrillation.
Dopamine should not be used in patients with pheochromocytoma.
Dopamine should not be administered in the presence of uncorrected tachyarrhythmias or ventricular fibrillation.
Careful monitoring required - Close monitoring of the following indices-urine flow, cardiac output and blood pressure - during Dopamine infusion is necessary as in the case of any adrenergic agent.
Avoid hypovolemia - Prior to treatment with Dopamine , hypovolemia should be fully corrected, if possible with either whole blood or plasma as indicated. Monitoring of central venous pressure of left ventricular filling pressure may be helpful in detecting and treating hypovolemia.
Hypoxia, Hypercapnia, Acidosis - These conditions which may also reduce the effectiveness and/or increase the incidence of adverse effects of dopamine, must be identified and corrected prior to, or concurrently with administration of dopamine.
Ventricular Arrhythmias - If an increased number of ectopic beats are observed, the dose should be reduced if possible.
Decreased Pulse Pressure - If a disproportionate rise in the diastolic pressure (i.e., a marked decrease in the pulse pressure) is observed in patients receiving Dopamine, the infusion rate should be decreased and the patient observed carefully for further evidence of predominant vasoconstrictor activity, unless such an effect is desired.
Hypotension - At lower infusion rates, if hypotension occurs, the infusion rate should be rapidly increased until adequate blood pressure is obtained. If hypotension persists, dopamine should be discontinued and a more potent vasoconstrictor agent such as norepinephrine should be administered.
Extravasation - Dopamine should be infused into a large vein whenever possible to prevent the possibility of extravasation into tissue adjacent to the infusion site. Extravasation may cause necrosis and sloughing of surrounding tissue. Large veins of the actecubital fossa are preferred to veins in the dorsum of the hand or ankle. Less suitable infusion sites should be used only if the patient's condition requires immediate attention. The physician should switch to more suitable sites as rapidly as possible. The infusion site should be continuously monitored for free flow.
Occlusive vascular disease - Patients with a history of occlusive vascular disease (for example, atheroscierosis, arterial embolism, and Raynaud's disease, cold injury, diabetic endarteritis, and Buergers disease) should be closely monitored for any changes in color or temperature of the skin in the extremities. If a change in skin color or temperature occurs and is thought to be the result of compromised circulation to the extremities, the benefits of continued Dopamine infusion should be weighed against the risk of possible necrosis. This condition may be reversed by either decreasing or discontinuing the rate of infusion.
Careful monitoring required - Close monitoring of the following indices-urine flow, cardiac output and blood pressure - during Dopamine infusion is necessary as in the case of any adrenergic agent.
Avoid hypovolemia - Prior to treatment with Dopamine , hypovolemia should be fully corrected, if possible with either whole blood or plasma as indicated. Monitoring of central venous pressure of left ventricular filling pressure may be helpful in detecting and treating hypovolemia.
Hypoxia, Hypercapnia, Acidosis - These conditions which may also reduce the effectiveness and/or increase the incidence of adverse effects of dopamine, must be identified and corrected prior to, or concurrently with administration of dopamine.
Ventricular Arrhythmias - If an increased number of ectopic beats are observed, the dose should be reduced if possible.
Decreased Pulse Pressure - If a disproportionate rise in the diastolic pressure (i.e., a marked decrease in the pulse pressure) is observed in patients receiving Dopamine, the infusion rate should be decreased and the patient observed carefully for further evidence of predominant vasoconstrictor activity, unless such an effect is desired.
Hypotension - At lower infusion rates, if hypotension occurs, the infusion rate should be rapidly increased until adequate blood pressure is obtained. If hypotension persists, dopamine should be discontinued and a more potent vasoconstrictor agent such as norepinephrine should be administered.
Extravasation - Dopamine should be infused into a large vein whenever possible to prevent the possibility of extravasation into tissue adjacent to the infusion site. Extravasation may cause necrosis and sloughing of surrounding tissue. Large veins of the actecubital fossa are preferred to veins in the dorsum of the hand or ankle. Less suitable infusion sites should be used only if the patient's condition requires immediate attention. The physician should switch to more suitable sites as rapidly as possible. The infusion site should be continuously monitored for free flow.
Occlusive vascular disease - Patients with a history of occlusive vascular disease (for example, atheroscierosis, arterial embolism, and Raynaud's disease, cold injury, diabetic endarteritis, and Buergers disease) should be closely monitored for any changes in color or temperature of the skin in the extremities. If a change in skin color or temperature occurs and is thought to be the result of compromised circulation to the extremities, the benefits of continued Dopamine infusion should be weighed against the risk of possible necrosis. This condition may be reversed by either decreasing or discontinuing the rate of infusion.
Careful monitoring required - Close monitoring of the following indices-urine flow, cardiac output and blood pressure - during Dopamine infusion is necessary as in the case of any adrenergic agent.
Avoid hypovolemia - Prior to treatment with Dopamine , hypovolemia should be fully corrected, if possible with either whole blood or plasma as indicated. Monitoring of central venous pressure of left ventricular filling pressure may be helpful in detecting and treating hypovolemia.
Hypoxia, Hypercapnia, Acidosis - These conditions which may also reduce the effectiveness and/or increase the incidence of adverse effects of dopamine, must be identified and corrected prior to, or concurrently with administration of dopamine.
Ventricular Arrhythmias - If an increased number of ectopic beats are observed, the dose should be reduced if possible.
Decreased Pulse Pressure - If a disproportionate rise in the diastolic pressure (i.e., a marked decrease in the pulse pressure) is observed in patients receiving Dopamine, the infusion rate should be decreased and the patient observed carefully for further evidence of predominant vasoconstrictor activity, unless such an effect is desired.
Hypotension - At lower infusion rates, if hypotension occurs, the infusion rate should be rapidly increased until adequate blood pressure is obtained. If hypotension persists, dopamine should be discontinued and a more potent vasoconstrictor agent such as norepinephrine should be administered.
Extravasation - Dopamine should be infused into a large vein whenever possible to prevent the possibility of extravasation into tissue adjacent to the infusion site. Extravasation may cause necrosis and sloughing of surrounding tissue. Large veins of the actecubital fossa are preferred to veins in the dorsum of the hand or ankle. Less suitable infusion sites should be used only if the patient's condition requires immediate attention. The physician should switch to more suitable sites as rapidly as possible. The infusion site should be continuously monitored for free flow.
Occlusive vascular disease - Patients with a history of occlusive vascular disease (for example, atheroscierosis, arterial embolism, and Raynaud's disease, cold injury, diabetic endarteritis, and Buergers disease) should be closely monitored for any changes in color or temperature of the skin in the extremities. If a change in skin color or temperature occurs and is thought to be the result of compromised circulation to the extremities, the benefits of continued Dopamine infusion should be weighed against the risk of possible necrosis. This condition may be reversed by either decreasing or discontinuing the rate of infusion.
Careful monitoring required - Close monitoring of the following indices-urine flow, cardiac output and blood pressure - during Dopamine infusion is necessary as in the case of any adrenergic agent.
Avoid hypovolemia - Prior to treatment with Dopamine , hypovolemia should be fully corrected, if possible with either whole blood or plasma as indicated. Monitoring of central venous pressure of left ventricular filling pressure may be helpful in detecting and treating hypovolemia.
Hypoxia, Hypercapnia, Acidosis - These conditions which may also reduce the effectiveness and/or increase the incidence of adverse effects of dopamine, must be identified and corrected prior to, or concurrently with administration of dopamine.
Ventricular Arrhythmias - If an increased number of ectopic beats are observed, the dose should be reduced if possible.
Decreased Pulse Pressure - If a disproportionate rise in the diastolic pressure (i.e., a marked decrease in the pulse pressure) is observed in patients receiving Dopamine, the infusion rate should be decreased and the patient observed carefully for further evidence of predominant vasoconstrictor activity, unless such an effect is desired.
Hypotension - At lower infusion rates, if hypotension occurs, the infusion rate should be rapidly increased until adequate blood pressure is obtained. If hypotension persists, dopamine should be discontinued and a more potent vasoconstrictor agent such as norepinephrine should be administered.
Extravasation - Dopamine should be infused into a large vein whenever possible to prevent the possibility of extravasation into tissue adjacent to the infusion site. Extravasation may cause necrosis and sloughing of surrounding tissue. Large veins of the actecubital fossa are preferred to veins in the dorsum of the hand or ankle. Less suitable infusion sites should be used only if the patient's condition requires immediate attention. The physician should switch to more suitable sites as rapidly as possible. The infusion site should be continuously monitored for free flow.
Occlusive vascular disease - Patients with a history of occlusive vascular disease (for example, atheroscierosis, arterial embolism, and Raynaud's disease, cold injury, diabetic endarteritis, and Buergers disease) should be closely monitored for any changes in color or temperature of the skin in the extremities. If a change in skin color or temperature occurs and is thought to be the result of compromised circulation to the extremities, the benefits of continued Dopamine infusion should be weighed against the risk of possible necrosis. This condition may be reversed by either decreasing or discontinuing the rate of infusion.
Careful monitoring required - Close monitoring of the following indices-urine flow, cardiac output and blood pressure - during Dopamine infusion is necessary as in the case of any adrenergic agent.
Avoid hypovolemia - Prior to treatment with Dopamine , hypovolemia should be fully corrected, if possible with either whole blood or plasma as indicated. Monitoring of central venous pressure of left ventricular filling pressure may be helpful in detecting and treating hypovolemia.
Hypoxia, Hypercapnia, Acidosis - These conditions which may also reduce the effectiveness and/or increase the incidence of adverse effects of dopamine, must be identified and corrected prior to, or concurrently with administration of dopamine.
Ventricular Arrhythmias - If an increased number of ectopic beats are observed, the dose should be reduced if possible.
Decreased Pulse Pressure - If a disproportionate rise in the diastolic pressure (i.e., a marked decrease in the pulse pressure) is observed in patients receiving Dopamine, the infusion rate should be decreased and the patient observed carefully for further evidence of predominant vasoconstrictor activity, unless such an effect is desired.
Hypotension - At lower infusion rates, if hypotension occurs, the infusion rate should be rapidly increased until adequate blood pressure is obtained. If hypotension persists, dopamine should be discontinued and a more potent vasoconstrictor agent such as norepinephrine should be administered.
Extravasation - Dopamine should be infused into a large vein whenever possible to prevent the possibility of extravasation into tissue adjacent to the infusion site. Extravasation may cause necrosis and sloughing of surrounding tissue. Large veins of the actecubital fossa are preferred to veins in the dorsum of the hand or ankle. Less suitable infusion sites should be used only if the patient's condition requires immediate attention. The physician should switch to more suitable sites as rapidly as possible. The infusion site should be continuously monitored for free flow.
Occlusive vascular disease - Patients with a history of occlusive vascular disease (for example, atheroscierosis, arterial embolism, and Raynaud's disease, cold injury, diabetic endarteritis, and Buergers disease) should be closely monitored for any changes in color or temperature of the skin in the extremities. If a change in skin color or temperature occurs and is thought to be the result of compromised circulation to the extremities, the benefits of continued Dopamine infusion should be weighed against the risk of possible necrosis. This condition may be reversed by either decreasing or discontinuing the rate of infusion.
Careful monitoring required - Close monitoring of the following indices-urine flow, cardiac output and blood pressure - during Dopamine infusion is necessary as in the case of any adrenergic agent.
Avoid hypovolemia - Prior to treatment with Dopamine , hypovolemia should be fully corrected, if possible with either whole blood or plasma as indicated. Monitoring of central venous pressure of left ventricular filling pressure may be helpful in detecting and treating hypovolemia.
Hypoxia, Hypercapnia, Acidosis - These conditions which may also reduce the effectiveness and/or increase the incidence of adverse effects of dopamine, must be identified and corrected prior to, or concurrently with administration of dopamine.
Ventricular Arrhythmias - If an increased number of ectopic beats are observed, the dose should be reduced if possible.
Decreased Pulse Pressure - If a disproportionate rise in the diastolic pressure (i.e., a marked decrease in the pulse pressure) is observed in patients receiving Dopamine, the infusion rate should be decreased and the patient observed carefully for further evidence of predominant vasoconstrictor activity, unless such an effect is desired.
Hypotension - At lower infusion rates, if hypotension occurs, the infusion rate should be rapidly increased until adequate blood pressure is obtained. If hypotension persists, dopamine should be discontinued and a more potent vasoconstrictor agent such as norepinephrine should be administered.
Extravasation - Dopamine should be infused into a large vein whenever possible to prevent the possibility of extravasation into tissue adjacent to the infusion site. Extravasation may cause necrosis and sloughing of surrounding tissue. Large veins of the actecubital fossa are preferred to veins in the dorsum of the hand or ankle. Less suitable infusion sites should be used only if the patient's condition requires immediate attention. The physician should switch to more suitable sites as rapidly as possible. The infusion site should be continuously monitored for free flow.
Occlusive vascular disease - Patients with a history of occlusive vascular disease (for example, atheroscierosis, arterial embolism, and Raynaud's disease, cold injury, diabetic endarteritis, and Buergers disease) should be closely monitored for any changes in color or temperature of the skin in the extremities. If a change in skin color or temperature occurs and is thought to be the result of compromised circulation to the extremities, the benefits of continued Dopamine infusion should be weighed against the risk of possible necrosis. This condition may be reversed by either decreasing or discontinuing the rate of infusion.
• droperidol ;
• epinephrine ;
• haloperidol ;
• midodrine ;
• phenytoin (dilantin);
• vasopressin ;
• a diuretic (water pill);
• an antidepressant such as amitriptyline , doxepin , nortriptyline , and others;
• a beta blocker such as atenolol , carvedilol , labetalol , metoprolol , nadolol , propranolol , sotalol , and others;
• cough or cold medicine that contains an antihistamine or decongestant;
• ergot medicine such as ergotamine , dihydroergotamine , ergonovine , or methylergonovine (Methergine);
• a phenothiazine such as chlorpromazine , fluphenazine , perphenazine , prochlorperazine , promethazine , thioridazine (Mellaril), or trifluoperazine ;
• droperidol ;
• epinephrine ;
• haloperidol ;
• midodrine ;
• phenytoin (dilantin);
• vasopressin ;
• a diuretic (water pill);
• an antidepressant such as amitriptyline , doxepin , nortriptyline , and others;
• a beta blocker such as atenolol , carvedilol , labetalol , metoprolol , nadolol , propranolol , sotalol , and others;
• cough or cold medicine that contains an antihistamine or decongestant;
• ergot medicine such as ergotamine , dihydroergotamine , ergonovine , or methylergonovine (Methergine);
• a phenothiazine such as chlorpromazine , fluphenazine , perphenazine , prochlorperazine , promethazine , thioridazine (Mellaril), or trifluoperazine ;
• droperidol ;
• epinephrine ;
• haloperidol ;
• midodrine ;
• phenytoin (dilantin);
• vasopressin ;
• a diuretic (water pill);
• an antidepressant such as amitriptyline , doxepin , nortriptyline , and others;
• a beta blocker such as atenolol , carvedilol , labetalol , metoprolol , nadolol , propranolol , sotalol , and others;
• cough or cold medicine that contains an antihistamine or decongestant;
• ergot medicine such as ergotamine , dihydroergotamine , ergonovine , or methylergonovine (Methergine);
• a phenothiazine such as chlorpromazine , fluphenazine , perphenazine , prochlorperazine , promethazine , thioridazine (Mellaril), or trifluoperazine ;
• droperidol ;
• epinephrine ;
• haloperidol ;
• midodrine ;
• phenytoin (dilantin);
• vasopressin ;
• a diuretic (water pill);
• an antidepressant such as amitriptyline , doxepin , nortriptyline , and others;
• a beta blocker such as atenolol , carvedilol , labetalol , metoprolol , nadolol , propranolol , sotalol , and others;
• cough or cold medicine that contains an antihistamine or decongestant;
• ergot medicine such as ergotamine , dihydroergotamine , ergonovine , or methylergonovine (Methergine);
• a phenothiazine such as chlorpromazine , fluphenazine , perphenazine , prochlorperazine , promethazine , thioridazine (Mellaril), or trifluoperazine ;
• droperidol ;
• epinephrine ;
• haloperidol ;
• midodrine ;
• phenytoin (dilantin);
• vasopressin ;
• a diuretic (water pill);
• an antidepressant such as amitriptyline , doxepin , nortriptyline , and others;
• a beta blocker such as atenolol , carvedilol , labetalol , metoprolol , nadolol , propranolol , sotalol , and others;
• cough or cold medicine that contains an antihistamine or decongestant;
• ergot medicine such as ergotamine , dihydroergotamine , ergonovine , or methylergonovine (Methergine);
• a phenothiazine such as chlorpromazine , fluphenazine , perphenazine , prochlorperazine , promethazine , thioridazine (Mellaril), or trifluoperazine ;
• chest pain;
• fast, slow, or pounding heartbeats;
• painful or difficult urination, blood in your urine;
• weakness, confusion, swelling in your feet or ankles, urinating less than usual or not at all;
• weak or shallow breathing;
• feeling like you might pass out, even while lying down;
• burning, pain, or swelling around the IV needle;
• cold feeling, numbness, or blue-colored appearance in your hands or feet; or
• darkening or skin changes in your hands or feet.
Less serious dopamine side effects may include:
• headache;
• feeling anxious;
• nausea, vomiting; or
• chills, goosebumps.
• chest pain;
• fast, slow, or pounding heartbeats;
• painful or difficult urination, blood in your urine;
• weakness, confusion, swelling in your feet or ankles, urinating less than usual or not at all;
• weak or shallow breathing;
• feeling like you might pass out, even while lying down;
• burning, pain, or swelling around the IV needle;
• cold feeling, numbness, or blue-colored appearance in your hands or feet; or
• darkening or skin changes in your hands or feet.
Less serious dopamine side effects may include:
• headache;
• feeling anxious;
• nausea, vomiting; or
• chills, goosebumps.
• chest pain;
• fast, slow, or pounding heartbeats;
• painful or difficult urination, blood in your urine;
• weakness, confusion, swelling in your feet or ankles, urinating less than usual or not at all;
• weak or shallow breathing;
• feeling like you might pass out, even while lying down;
• burning, pain, or swelling around the IV needle;
• cold feeling, numbness, or blue-colored appearance in your hands or feet; or
• darkening or skin changes in your hands or feet.
Less serious dopamine side effects may include:
• headache;
• feeling anxious;
• nausea, vomiting; or
• chills, goosebumps.
• chest pain;
• fast, slow, or pounding heartbeats;
• painful or difficult urination, blood in your urine;
• weakness, confusion, swelling in your feet or ankles, urinating less than usual or not at all;
• weak or shallow breathing;
• feeling like you might pass out, even while lying down;
• burning, pain, or swelling around the IV needle;
• cold feeling, numbness, or blue-colored appearance in your hands or feet; or
• darkening or skin changes in your hands or feet.
Less serious dopamine side effects may include:
• headache;
• feeling anxious;
• nausea, vomiting; or
• chills, goosebumps.
• chest pain;
• fast, slow, or pounding heartbeats;
• painful or difficult urination, blood in your urine;
• weakness, confusion, swelling in your feet or ankles, urinating less than usual or not at all;
• weak or shallow breathing;
• feeling like you might pass out, even while lying down;
• burning, pain, or swelling around the IV needle;
• cold feeling, numbness, or blue-colored appearance in your hands or feet; or
• darkening or skin changes in your hands or feet.
Less serious dopamine side effects may include:
• headache;
• feeling anxious;
• nausea, vomiting; or
• chills, goosebumps.
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
• Injection 200mg/5ml: Box of 5 ampoules
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>• Injection 200mg/5ml: Box of 5 ampoules
) [#title] => [#description] => [#children] =>• Injection 200mg/5ml: Box of 5 ampoules
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_packing [#title] => Packing [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>• Injection 200mg/5ml: Box of 5 ampoules
[#printed] => 1 ) [#title] => [#description] => [#children] =>• Injection 200mg/5ml: Box of 5 ampoules
DOPADIC®
Injection 200mg/5ml
Cardiovascular Drugs
Inotropic Agents
Category C
Dopamine is a natural catecholamine formed by the decarboxylation of 3,4-dihydroxyphenylalanine (DOPA). It is a precursor to norepinephrine in noradrenergic nerves and is also a neurotransmitter in certain areas of the central nervous system, especially in the nigrostriatal tract, and in a few peripheral sympathetic nerves.
Dopamine produces positive chronotropic and inotropic effects on the myocardium, resulting in increased heart rate and cardiac contractility. This is accomplished directly by exerting an agonist action on beta-adrenoceptors and indirectly by causing release of norepinephrine from storage sites in sympathetic nerve endings.
Dopamine (dopamine hydrochloride) 's onset of action occurs within five minutes of intravenous administration, and with dopamine (dopamine hydrochloride) 's plasma half-life of about two minutes, the duration of action is less than ten minutes. If monoamine oxidase (MAO) inhibitors are present, however, the duration may increase to one hour. The drug is widely distributed in the body but does not cross the blood-brain barrier to a significant extent. Dopamine (dopamine hydrochloride) is metabolized in the liver, kidney, and plasma by MAO and catechol-O-methyltransferase to the inactive compounds homovanillic acid (HVA) and 3,4-dihydroxyphenylacetic acid. About 25% of the dose is taken up into specialized neurosecretory vesicles (the adrenergic nerve terminals), where it is hydroxylated to form norepinephrine. It has been reported that about 80% of the drug is excreted in the urine within 24 hours, primarily as HVA and its sulfate and glucuronide conjugates and as 3,4-dihydroxyphenylacetic acid. A very small portion is excreted unchanged.
Dopamine is indicated for the correction of hemodynamic imbalances present in the shock syndrome due to myocardial infarctions, trauma, endotoxic septicemia, open heart surgery, renal failure, and chronic cardiac decompensation as in congestive failure.
Dopamine should not be used in patients with pheochromocytoma.
Dopamine should not be administered in the presence of uncorrected tachyarrhythmias or ventricular fibrillation.
Careful monitoring required - Close monitoring of the following indices-urine flow, cardiac output and blood pressure - during Dopamine infusion is necessary as in the case of any adrenergic agent.
Avoid hypovolemia - Prior to treatment with Dopamine , hypovolemia should be fully corrected, if possible with either whole blood or plasma as indicated. Monitoring of central venous pressure of left ventricular filling pressure may be helpful in detecting and treating hypovolemia.
Hypoxia, Hypercapnia, Acidosis - These conditions which may also reduce the effectiveness and/or increase the incidence of adverse effects of dopamine, must be identified and corrected prior to, or concurrently with administration of dopamine.
Ventricular Arrhythmias - If an increased number of ectopic beats are observed, the dose should be reduced if possible.
Decreased Pulse Pressure - If a disproportionate rise in the diastolic pressure (i.e., a marked decrease in the pulse pressure) is observed in patients receiving Dopamine, the infusion rate should be decreased and the patient observed carefully for further evidence of predominant vasoconstrictor activity, unless such an effect is desired.
Hypotension - At lower infusion rates, if hypotension occurs, the infusion rate should be rapidly increased until adequate blood pressure is obtained. If hypotension persists, dopamine should be discontinued and a more potent vasoconstrictor agent such as norepinephrine should be administered.
Extravasation - Dopamine should be infused into a large vein whenever possible to prevent the possibility of extravasation into tissue adjacent to the infusion site. Extravasation may cause necrosis and sloughing of surrounding tissue. Large veins of the actecubital fossa are preferred to veins in the dorsum of the hand or ankle. Less suitable infusion sites should be used only if the patient's condition requires immediate attention. The physician should switch to more suitable sites as rapidly as possible. The infusion site should be continuously monitored for free flow.
Occlusive vascular disease - Patients with a history of occlusive vascular disease (for example, atheroscierosis, arterial embolism, and Raynaud's disease, cold injury, diabetic endarteritis, and Buergers disease) should be closely monitored for any changes in color or temperature of the skin in the extremities. If a change in skin color or temperature occurs and is thought to be the result of compromised circulation to the extremities, the benefits of continued Dopamine infusion should be weighed against the risk of possible necrosis. This condition may be reversed by either decreasing or discontinuing the rate of infusion.
• droperidol ;
• epinephrine ;
• haloperidol ;
• midodrine ;
• phenytoin (dilantin);
• vasopressin ;
• a diuretic (water pill);
• an antidepressant such as amitriptyline , doxepin , nortriptyline , and others;
• a beta blocker such as atenolol , carvedilol , labetalol , metoprolol , nadolol , propranolol , sotalol , and others;
• cough or cold medicine that contains an antihistamine or decongestant;
• ergot medicine such as ergotamine , dihydroergotamine , ergonovine , or methylergonovine (Methergine);
• a phenothiazine such as chlorpromazine , fluphenazine , perphenazine , prochlorperazine , promethazine , thioridazine (Mellaril), or trifluoperazine ;
• chest pain;
• fast, slow, or pounding heartbeats;
• painful or difficult urination, blood in your urine;
• weakness, confusion, swelling in your feet or ankles, urinating less than usual or not at all;
• weak or shallow breathing;
• feeling like you might pass out, even while lying down;
• burning, pain, or swelling around the IV needle;
• cold feeling, numbness, or blue-colored appearance in your hands or feet; or
• darkening or skin changes in your hands or feet.
Less serious dopamine side effects may include:
• headache;
• feeling anxious;
• nausea, vomiting; or
• chills, goosebumps.
• Store below 30 C°
• Protect from light and freezing
• Injection 200mg/5ml: Box of 5 ampoules