Caspian Products
- Ampoules
- Anlagesics, Anti-inflammatory Drugs
- Antimyasthenics ,Muscle Relaxants
- Antiparkinson Drugs, Antidepressants,Antiepileptics, Anxiolytic Sedative, Hypnotics and Antipsychotics
- Hormonal Drugs
- Antihistamines, Bronchodilators
- Cardiovascular Drugs,Electrolytes
- Corticosteroids
- General Anaesthetics, Local Anaesthetics
- Antibacterials
- Gastrointestinal Drugs
- Nutritional Agents and Vitamins
- Antagonists
- Suppository
- Syrups & Oral Solutions
- Ointments, Creams & Gels
- Vial
- Prefilled Syringe
Octreotide
Pharmacology
Octreotide acetate exerts pharmacologic actions similar to the natural hormone, somatostatin. It is an even more potent inhibitor of growth hormone, glucagon, and insulin than somatostatin. Like somatostatin, it also suppresses LH response to GnRH, decreases splanchnic blood flow, and inhibits release of serotonin, gastrin, vasoactive intestinal peptide, secretin, motilin, and pancreatic polypeptide.
Pharmacokinetics:
After subcutaneous injection, Octreotide is absorbed rapidly and completely from the injection site. Peak concentrations of 5.2 ng/mL (100-mcg dose) were reached 0.4 hours after dosing. Using a specific radioimmunoassay, intravenous and subcutaneous doses were found to be bioequivalent. Peak concentrations and area under the curve values were dose proportional after intravenous single doses up to 200 mcg and subcutaneous single doses up to 500 mcg and after subcutaneous multiple doses up to 500 mcg t.i.d. (1500 mcg/day).
In healthy volunteers the distribution of Octreotide from plasma was rapid (tα1/2=0.2 h), the volume of distribution (Vdss) was estimated to be 13.6 L, and the total body clearance ranged from 7 L/hr to 10 L/hr. In blood, the distribution into the erythrocytes was found to be negligible and about 65% was bound in the plasma in a concentration-independent manner. Binding was mainly to lipoprotein and, to a lesser extent, to albumin.
The elimination of Octreotide from plasma had an apparent half-life of 1.7 to 1.9 hours compared with 1 to 3 minutes with the natural hormone. The duration of action of Octreotide acetate is variable but extends up to 12 hours depending upon the type of tumor. About 32% of the dose is excreted unchanged into the urine. In an elderly population, dose adjustments may be necessary due to a significant increase in the half-life (46%) and a significant decrease in the clearance (26%) of the drug.
In patients with acromegaly, the pharmacokinetics differ somewhat from those in healthy volunteers. A mean peak concentration of 2.8 ng/mL (100-mcg dose) was reached in 0.7 hours after subcutaneous dosing. The volume of distribution (Vdss) was estimated to be 21.6 ± 8.5 L and the total body clearance was increased to 18 L/h. The mean percent of the drug bound was 41.2%. The disposition and elimination half-lives were similar to normals.
In patients with renal impairment the elimination of Octreotide from plasma was prolonged and total body clearance reduced. In mild renal impairment (ClCR40 to 60 mL/min) Octreotide t1/2 was 2.4 hours and total body clearance was 8.8 L/hr, in moderate impairment (ClCR10 to 39 mL/min) t1/2 was 3.0 hours and total body clearance 7.3 L/hr, and in severely renally impaired patients not requiring dialysis (ClCR<10 mL/min) t1/2 was 3.1 hours and total body clearance was 7.6 L/hr. In patients with severe renal failure requiring dialysis, total body clearance was reduced to about half that found in healthy subjects (from approximately 10 L/hr to 4.5 L/hr).
Patients with liver cirrhosis showed prolonged elimination of drug, with Octreotide t1/2 increasing to 3.7 hr and total body clearance decreasing to 5.9 L/hr, whereas patients with fatty liver disease showed t1/2 increased to 3.4 hr and total body clearance of 8.2 L/hr.
Indications:
Acromegaly
Octreotide acetate is indicated to reduce blood levels of growth hormone and IGF-I (somatomedin C) in acromegaly patients who have had inadequate response to or cannot be treated with surgical resection, pituitary irradiation, and bromocriptine mesylate at maximally tolerated doses. The goal is to achieve normalization of growth hormone and IGF-I (somatomedin C) levels. In patients with acromegaly, Octreotide acetate reduces growth hormone to within normal ranges in 50% of patients and reduces IGF-I (somatomedin C) to within normal ranges in 50% to 60% of patients. Since the effects of pituitary irradiation may not become maximal for several years, adjunctive therapy with Octreotide acetate to reduce blood levels of growth hormone and IGF-I (somatomedin C) offers potential benefit before the effects of irradiation are manifested.
Improvement in clinical signs and symptoms or reduction in tumor size or rate of growth were not shown in clinical trials performed with Octreotide acetate; these trials were not optimally designed to detect such effects.
Carcinoid Tumors
Octreotide acetate is indicated for the symptomatic treatment of patients with metastatic carcinoid tumors where it suppresses or inhibits the severe diarrhea and flushing episodes associated with the disease.
Octreotide acetate studies were not designed to show an effect on the size, rate of growth or development of metastases.
Vasoactive Intestinal Peptide Tumors (VIPomas)
Octreotide acetate is indicated for the treatment of the profuse watery diarrhea associated with VIP-secreting tumors. Octreotide acetate studies were not designed to show an effect on the size, rate of growth or development of metastases.
Contraindications:
Known hypersensitivity to octreotide or any ingredient in the formulation.
Precautions:
Octreotide acetate alters the balance between the counter-regulatory hormones, insulin, glucagon and growth hormone, which may result in hypoglycemia or hyperglycemia. Octreotide acetate also suppresses secretion of thyroid stimulating hormone, which may result in hypothyroidism. Cardiac conduction abnormalities have also occurred during treatment with Octreotide acetate. However, the incidence of these adverse events during long-term therapy was determined vigorously only in acromegaly patients who, due to their underlying disease and/or the subsequent treatment they receive, are at an increased risk for the development of diabetes mellitus, hypothyroidism, and cardiovascular disease. Although the degree to which these abnormalities are related to Octreotide acetate therapy is not clear, new abnormalities of glycemic control, thyroid function and ECG developed during Octreotide acetate therapy as described below.
Drug Interactions:
Octreotide acetate has been associated with alterations in nutrient absorption, so it may have an effect on absorption of orally administered drugs. Concomitant administration of Octreotide acetate with cyclosporine may decrease blood levels of cyclosporine and result in transplant rejection.
Patients receiving insulin, oral hypoglycemic agents, beta blockers, calcium channel blockers, or agents to control fluid and electrolyte balance, may require dose adjustments of these therapeutic agents.
Concomitant administration of Octreotide and bromocriptine increases the availability of bromocriptine. Limited published data indicate that somatostatin analogs might decrease the metabolic clearance of compounds known to be metabolized by cytochrome P450 enzymes, which may be due to the suppression of growth hormones. Since it cannot be excluded that Octreotide may have this effect, other drugs mainly metabolized by CYP3A4 and which have a low therapeutic index (e.g., quinidine, terfenadine) should therefore be used with caution.
Side Effects:
Gallbladder Abnormalities
Gallbladder abnormalities, especially stones and/or biliary sludge, frequently develop in patients on chronic Octreotide acetate therapy .
Cardiac
In acromegalics, sinus bradycardia (<50 bpm) developed in 25%; conduction abnormalities occurred in 10% and arrhythmias developed in 9% of patients during Octreotide acetate therapy.
Gastrointestinal
Diarrhea, loose stools, nausea and abdominal discomfort were each seen in 34% to 61% of acromegalic patients in U.S. studies although only 2.6% of the patients discontinued therapy due to these symptoms. These symptoms were seen in 5% to 10% of patients with other disorders.
The frequency of these symptoms was not dose-related, but diarrhea and abdominal discomfort generally resolved more quickly in patients treated with 300 mcg/day than in those treated with 750 mcg/day. Vomiting, flatulence, abnormal stools, abdominal distention, and constipation were each seen in less than 10% of patients.
In rare instances, gastrointestinal side effects may resemble acute intestinal obstruction, with progressive abdominal distension, severe epigastric pain, abdominal tenderness and guarding.
Hypo/Hyperglycemia
Hypoglycemia and hyperglycemia occurred in 3% and 16% of acromegalic patients, respectively, but only in about 1.5% of other patients. Symptoms of hypoglycemia were noted in approximately 2% of patients.
Hypothyroidism
In acromegalics, biochemical hypothyroidism alone occurred in 12% while goiter occurred in 6% during Octreotide acetate therapy. In patients without acromegaly, hypothyroidism has only been reported in several isolated patients and goiter has not been reported.
Other Adverse Events
Pain on injection was reported in 7.7%, headache in 6% and dizziness in 5%. Pancreatitis was also observed.
Storage:
• Store below 30 C°
• Protect from light and freezing
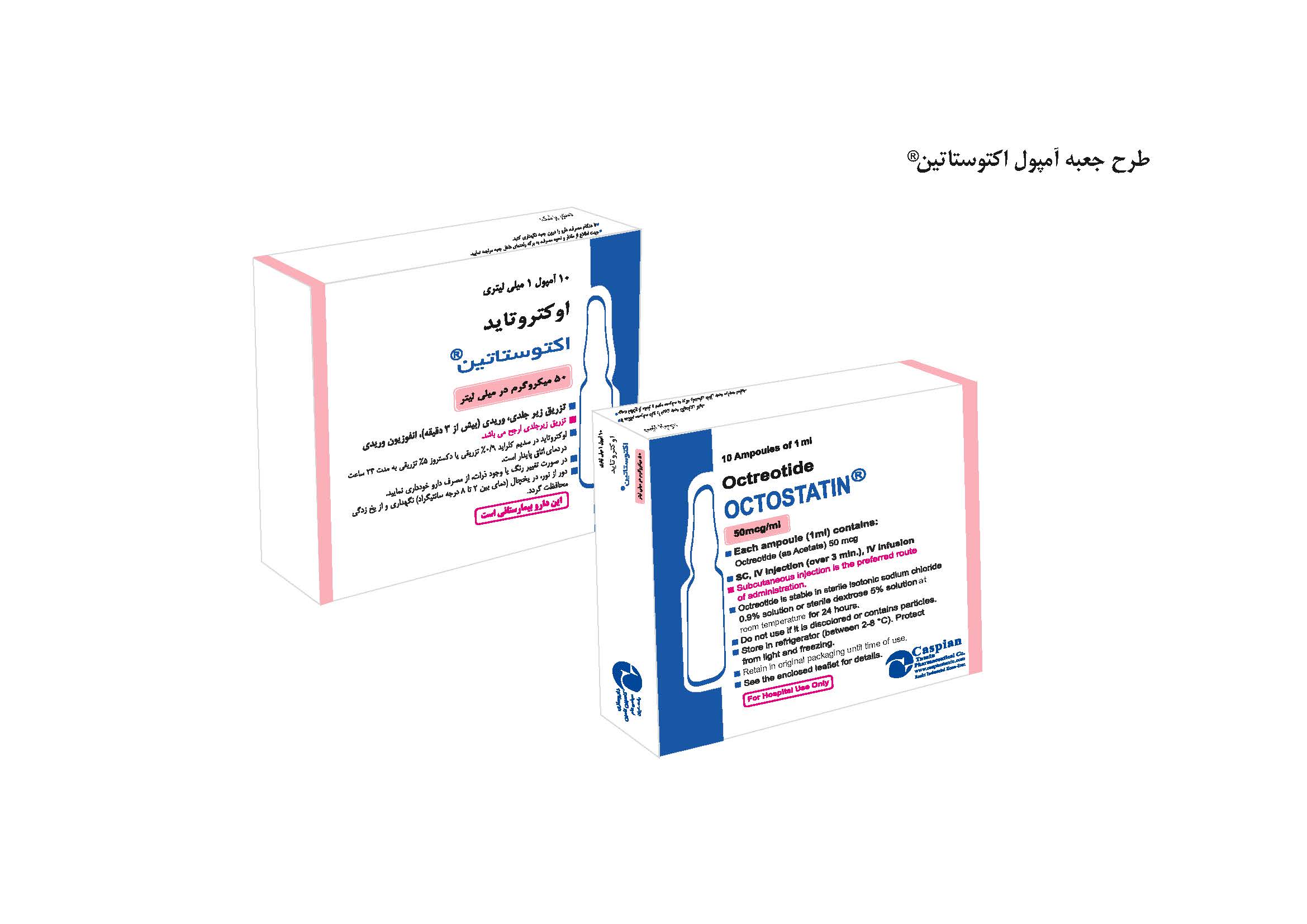
Packing:
• Injection 50 mcg/1ml: Box of 5Ampoules
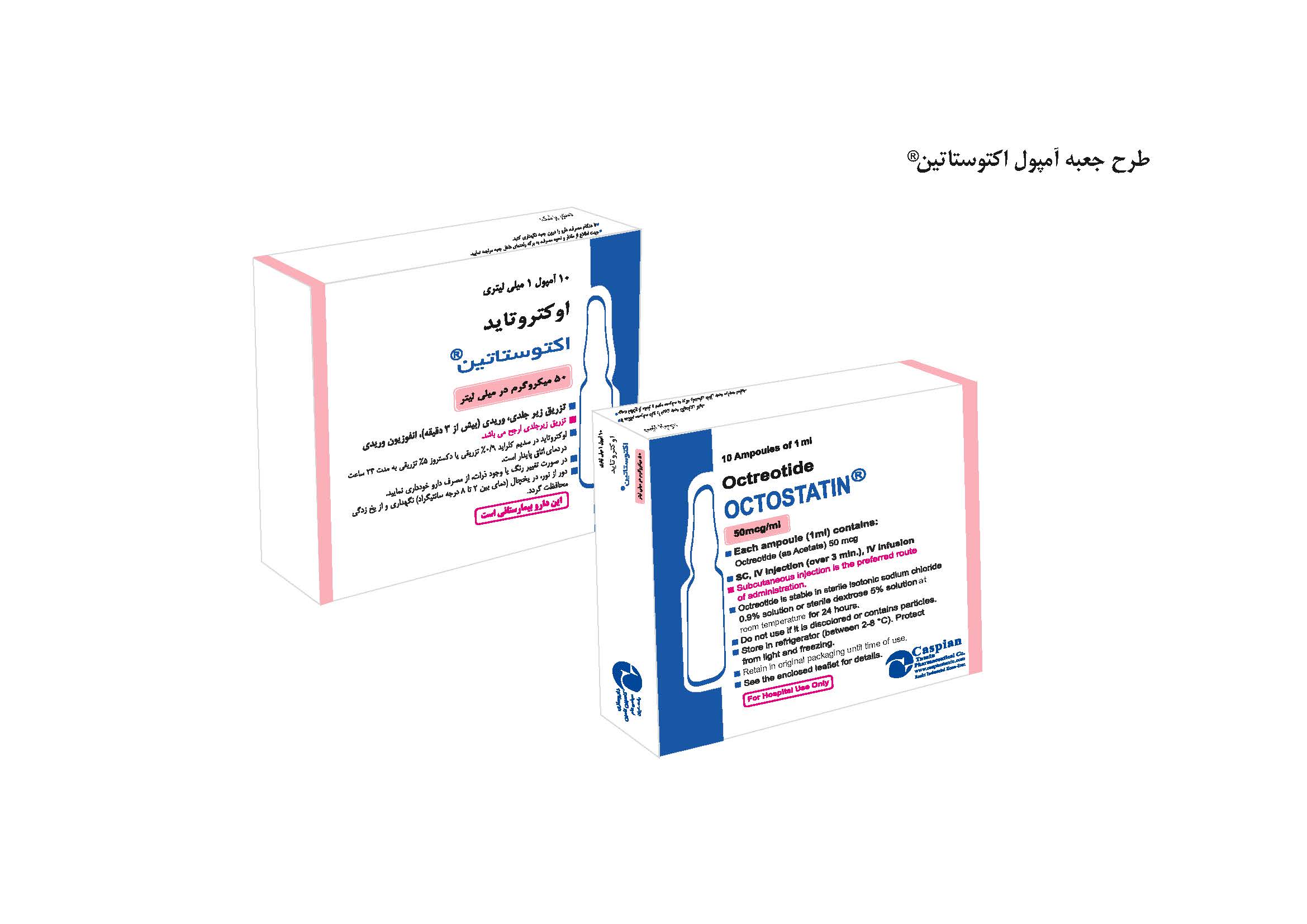
OCTOSTATIN®
Injection 50 mcg/1ml
Pituitary Hormones
Somatostatin Analogue
Category B
Octreotide acetate exerts pharmacologic actions similar to the natural hormone, somatostatin. It is an even more potent inhibitor of growth hormone, glucagon, and insulin than somatostatin. Like somatostatin, it also suppresses LH response to GnRH, decreases splanchnic blood flow, and inhibits release of serotonin, gastrin, vasoactive intestinal peptide, secretin, motilin, and pancreatic polypeptide.
After subcutaneous injection, Octreotide is absorbed rapidly and completely from the injection site. Peak concentrations of 5.2 ng/mL (100-mcg dose) were reached 0.4 hours after dosing. Using a specific radioimmunoassay, intravenous and subcutaneous doses were found to be bioequivalent. Peak concentrations and area under the curve values were dose proportional after intravenous single doses up to 200 mcg and subcutaneous single doses up to 500 mcg and after subcutaneous multiple doses up to 500 mcg t.i.d. (1500 mcg/day).
In healthy volunteers the distribution of Octreotide from plasma was rapid (tα1/2=0.2 h), the volume of distribution (Vdss) was estimated to be 13.6 L, and the total body clearance ranged from 7 L/hr to 10 L/hr. In blood, the distribution into the erythrocytes was found to be negligible and about 65% was bound in the plasma in a concentration-independent manner. Binding was mainly to lipoprotein and, to a lesser extent, to albumin.
The elimination of Octreotide from plasma had an apparent half-life of 1.7 to 1.9 hours compared with 1 to 3 minutes with the natural hormone. The duration of action of Octreotide acetate is variable but extends up to 12 hours depending upon the type of tumor. About 32% of the dose is excreted unchanged into the urine. In an elderly population, dose adjustments may be necessary due to a significant increase in the half-life (46%) and a significant decrease in the clearance (26%) of the drug.
In patients with acromegaly, the pharmacokinetics differ somewhat from those in healthy volunteers. A mean peak concentration of 2.8 ng/mL (100-mcg dose) was reached in 0.7 hours after subcutaneous dosing. The volume of distribution (Vdss) was estimated to be 21.6 ± 8.5 L and the total body clearance was increased to 18 L/h. The mean percent of the drug bound was 41.2%. The disposition and elimination half-lives were similar to normals.
In patients with renal impairment the elimination of Octreotide from plasma was prolonged and total body clearance reduced. In mild renal impairment (ClCR40 to 60 mL/min) Octreotide t1/2 was 2.4 hours and total body clearance was 8.8 L/hr, in moderate impairment (ClCR10 to 39 mL/min) t1/2 was 3.0 hours and total body clearance 7.3 L/hr, and in severely renally impaired patients not requiring dialysis (ClCR<10 mL/min) t1/2 was 3.1 hours and total body clearance was 7.6 L/hr. In patients with severe renal failure requiring dialysis, total body clearance was reduced to about half that found in healthy subjects (from approximately 10 L/hr to 4.5 L/hr).
Patients with liver cirrhosis showed prolonged elimination of drug, with Octreotide t1/2 increasing to 3.7 hr and total body clearance decreasing to 5.9 L/hr, whereas patients with fatty liver disease showed t1/2 increased to 3.4 hr and total body clearance of 8.2 L/hr.
Acromegaly
Octreotide acetate is indicated to reduce blood levels of growth hormone and IGF-I (somatomedin C) in acromegaly patients who have had inadequate response to or cannot be treated with surgical resection, pituitary irradiation, and bromocriptine mesylate at maximally tolerated doses. The goal is to achieve normalization of growth hormone and IGF-I (somatomedin C) levels. In patients with acromegaly, Octreotide acetate reduces growth hormone to within normal ranges in 50% of patients and reduces IGF-I (somatomedin C) to within normal ranges in 50% to 60% of patients. Since the effects of pituitary irradiation may not become maximal for several years, adjunctive therapy with Octreotide acetate to reduce blood levels of growth hormone and IGF-I (somatomedin C) offers potential benefit before the effects of irradiation are manifested.
Improvement in clinical signs and symptoms or reduction in tumor size or rate of growth were not shown in clinical trials performed with Octreotide acetate; these trials were not optimally designed to detect such effects.
Carcinoid Tumors
Octreotide acetate is indicated for the symptomatic treatment of patients with metastatic carcinoid tumors where it suppresses or inhibits the severe diarrhea and flushing episodes associated with the disease.
Octreotide acetate studies were not designed to show an effect on the size, rate of growth or development of metastases.
Vasoactive Intestinal Peptide Tumors (VIPomas)
Octreotide acetate is indicated for the treatment of the profuse watery diarrhea associated with VIP-secreting tumors. Octreotide acetate studies were not designed to show an effect on the size, rate of growth or development of metastases.
Known hypersensitivity to octreotide or any ingredient in the formulation.
Octreotide acetate alters the balance between the counter-regulatory hormones, insulin, glucagon and growth hormone, which may result in hypoglycemia or hyperglycemia. Octreotide acetate also suppresses secretion of thyroid stimulating hormone, which may result in hypothyroidism. Cardiac conduction abnormalities have also occurred during treatment with Octreotide acetate. However, the incidence of these adverse events during long-term therapy was determined vigorously only in acromegaly patients who, due to their underlying disease and/or the subsequent treatment they receive, are at an increased risk for the development of diabetes mellitus, hypothyroidism, and cardiovascular disease. Although the degree to which these abnormalities are related to Octreotide acetate therapy is not clear, new abnormalities of glycemic control, thyroid function and ECG developed during Octreotide acetate therapy as described below.
Octreotide acetate has been associated with alterations in nutrient absorption, so it may have an effect on absorption of orally administered drugs. Concomitant administration of Octreotide acetate with cyclosporine may decrease blood levels of cyclosporine and result in transplant rejection.
Patients receiving insulin, oral hypoglycemic agents, beta blockers, calcium channel blockers, or agents to control fluid and electrolyte balance, may require dose adjustments of these therapeutic agents.
Concomitant administration of Octreotide and bromocriptine increases the availability of bromocriptine. Limited published data indicate that somatostatin analogs might decrease the metabolic clearance of compounds known to be metabolized by cytochrome P450 enzymes, which may be due to the suppression of growth hormones. Since it cannot be excluded that Octreotide may have this effect, other drugs mainly metabolized by CYP3A4 and which have a low therapeutic index (e.g., quinidine, terfenadine) should therefore be used with caution.
Gallbladder Abnormalities
Gallbladder abnormalities, especially stones and/or biliary sludge, frequently develop in patients on chronic Octreotide acetate therapy .
Cardiac
In acromegalics, sinus bradycardia (<50 bpm) developed in 25%; conduction abnormalities occurred in 10% and arrhythmias developed in 9% of patients during Octreotide acetate therapy.
Gastrointestinal
Diarrhea, loose stools, nausea and abdominal discomfort were each seen in 34% to 61% of acromegalic patients in U.S. studies although only 2.6% of the patients discontinued therapy due to these symptoms. These symptoms were seen in 5% to 10% of patients with other disorders.
The frequency of these symptoms was not dose-related, but diarrhea and abdominal discomfort generally resolved more quickly in patients treated with 300 mcg/day than in those treated with 750 mcg/day. Vomiting, flatulence, abnormal stools, abdominal distention, and constipation were each seen in less than 10% of patients.
In rare instances, gastrointestinal side effects may resemble acute intestinal obstruction, with progressive abdominal distension, severe epigastric pain, abdominal tenderness and guarding.
Hypo/Hyperglycemia
Hypoglycemia and hyperglycemia occurred in 3% and 16% of acromegalic patients, respectively, but only in about 1.5% of other patients. Symptoms of hypoglycemia were noted in approximately 2% of patients.
Hypothyroidism
In acromegalics, biochemical hypothyroidism alone occurred in 12% while goiter occurred in 6% during Octreotide acetate therapy. In patients without acromegaly, hypothyroidism has only been reported in several isolated patients and goiter has not been reported.
Other Adverse Events
Pain on injection was reported in 7.7%, headache in 6% and dizziness in 5%. Pancreatitis was also observed.
• Store below 30 C°
• Protect from light and freezing
• Injection 50 mcg/1ml: Box of 5Ampoules
 )
)
[field_administration_and_dosage] => Array
(
[0] => Array
(
[value] =>
[format] =>
[safe] =>
[view] =>
)
)
[field_brand_name] => Array
(
[0] => Array
(
[value] => OCTOSTATIN®
[format] => 1
[safe] =>
)
)
[field_administration_and_dosage] => Array
(
[0] => Array
(
[value] =>
[format] =>
[safe] =>
[view] =>
)
)
[field_brand_name] => Array
(
[0] => Array
(
[value] => OCTOSTATIN®
[format] => 1
[safe] => OCTOSTATIN®
[view] =>OCTOSTATIN®
) ) [field_contraindications] => Array ( [0] => Array ( [value] => Known hypersensitivity to octreotide or any ingredient in the formulation. [format] => 1 [safe] =>Known hypersensitivity to octreotide or any ingredient in the formulation.
[view] =>Known hypersensitivity to octreotide or any ingredient in the formulation.
) ) [field_dosage_form] => Array ( [0] => Array ( [value] => Injection 50 mcg/1ml [format] => 1 [safe] =>Injection 50 mcg/1ml
[view] =>Injection 50 mcg/1ml
) ) [field_drug_interactions] => Array ( [0] => Array ( [value] => Octreotide acetate has been associated with alterations in nutrient absorption, so it may have an effect on absorption of orally administered drugs. Concomitant administration of Octreotide acetate with cyclosporine may decrease blood levels of cyclosporine and result in transplant rejection. Patients receiving insulin, oral hypoglycemic agents, beta blockers, calcium channel blockers, or agents to control fluid and electrolyte balance, may require dose adjustments of these therapeutic agents. Concomitant administration of Octreotide and bromocriptine increases the availability of bromocriptine. Limited published data indicate that somatostatin analogs might decrease the metabolic clearance of compounds known to be metabolized by cytochrome P450 enzymes, which may be due to the suppression of growth hormones. Since it cannot be excluded that Octreotide may have this effect, other drugs mainly metabolized by CYP3A4 and which have a low therapeutic index (e.g., quinidine, terfenadine) should therefore be used with caution. [format] => 1 [safe] =>Octreotide acetate has been associated with alterations in nutrient absorption, so it may have an effect on absorption of orally administered drugs. Concomitant administration of Octreotide acetate with cyclosporine may decrease blood levels of cyclosporine and result in transplant rejection.
Patients receiving insulin, oral hypoglycemic agents, beta blockers, calcium channel blockers, or agents to control fluid and electrolyte balance, may require dose adjustments of these therapeutic agents.
Concomitant administration of Octreotide and bromocriptine increases the availability of bromocriptine. Limited published data indicate that somatostatin analogs might decrease the metabolic clearance of compounds known to be metabolized by cytochrome P450 enzymes, which may be due to the suppression of growth hormones. Since it cannot be excluded that Octreotide may have this effect, other drugs mainly metabolized by CYP3A4 and which have a low therapeutic index (e.g., quinidine, terfenadine) should therefore be used with caution.
Octreotide acetate has been associated with alterations in nutrient absorption, so it may have an effect on absorption of orally administered drugs. Concomitant administration of Octreotide acetate with cyclosporine may decrease blood levels of cyclosporine and result in transplant rejection.
Patients receiving insulin, oral hypoglycemic agents, beta blockers, calcium channel blockers, or agents to control fluid and electrolyte balance, may require dose adjustments of these therapeutic agents.
Concomitant administration of Octreotide and bromocriptine increases the availability of bromocriptine. Limited published data indicate that somatostatin analogs might decrease the metabolic clearance of compounds known to be metabolized by cytochrome P450 enzymes, which may be due to the suppression of growth hormones. Since it cannot be excluded that Octreotide may have this effect, other drugs mainly metabolized by CYP3A4 and which have a low therapeutic index (e.g., quinidine, terfenadine) should therefore be used with caution.
Acromegaly
Octreotide acetate is indicated to reduce blood levels of growth hormone and IGF-I (somatomedin C) in acromegaly patients who have had inadequate response to or cannot be treated with surgical resection, pituitary irradiation, and bromocriptine mesylate at maximally tolerated doses. The goal is to achieve normalization of growth hormone and IGF-I (somatomedin C) levels. In patients with acromegaly, Octreotide acetate reduces growth hormone to within normal ranges in 50% of patients and reduces IGF-I (somatomedin C) to within normal ranges in 50% to 60% of patients. Since the effects of pituitary irradiation may not become maximal for several years, adjunctive therapy with Octreotide acetate to reduce blood levels of growth hormone and IGF-I (somatomedin C) offers potential benefit before the effects of irradiation are manifested.
Improvement in clinical signs and symptoms or reduction in tumor size or rate of growth were not shown in clinical trials performed with Octreotide acetate; these trials were not optimally designed to detect such effects.
Carcinoid Tumors
Octreotide acetate is indicated for the symptomatic treatment of patients with metastatic carcinoid tumors where it suppresses or inhibits the severe diarrhea and flushing episodes associated with the disease.
Octreotide acetate studies were not designed to show an effect on the size, rate of growth or development of metastases.
Vasoactive Intestinal Peptide Tumors (VIPomas)
Octreotide acetate is indicated for the treatment of the profuse watery diarrhea associated with VIP-secreting tumors. Octreotide acetate studies were not designed to show an effect on the size, rate of growth or development of metastases.
Acromegaly
Octreotide acetate is indicated to reduce blood levels of growth hormone and IGF-I (somatomedin C) in acromegaly patients who have had inadequate response to or cannot be treated with surgical resection, pituitary irradiation, and bromocriptine mesylate at maximally tolerated doses. The goal is to achieve normalization of growth hormone and IGF-I (somatomedin C) levels. In patients with acromegaly, Octreotide acetate reduces growth hormone to within normal ranges in 50% of patients and reduces IGF-I (somatomedin C) to within normal ranges in 50% to 60% of patients. Since the effects of pituitary irradiation may not become maximal for several years, adjunctive therapy with Octreotide acetate to reduce blood levels of growth hormone and IGF-I (somatomedin C) offers potential benefit before the effects of irradiation are manifested.
Improvement in clinical signs and symptoms or reduction in tumor size or rate of growth were not shown in clinical trials performed with Octreotide acetate; these trials were not optimally designed to detect such effects.
Carcinoid Tumors
Octreotide acetate is indicated for the symptomatic treatment of patients with metastatic carcinoid tumors where it suppresses or inhibits the severe diarrhea and flushing episodes associated with the disease.
Octreotide acetate studies were not designed to show an effect on the size, rate of growth or development of metastases.
Vasoactive Intestinal Peptide Tumors (VIPomas)
Octreotide acetate is indicated for the treatment of the profuse watery diarrhea associated with VIP-secreting tumors. Octreotide acetate studies were not designed to show an effect on the size, rate of growth or development of metastases.
Acromegaly
Octreotide acetate is indicated to reduce blood levels of growth hormone and IGF-I (somatomedin C) in acromegaly patients who have had inadequate response to or cannot be treated with surgical resection, pituitary irradiation, and bromocriptine mesylate at maximally tolerated doses. The goal is to achieve normalization of growth hormone and IGF-I (somatomedin C) levels. In patients with acromegaly, Octreotide acetate reduces growth hormone to within normal ranges in 50% of patients and reduces IGF-I (somatomedin C) to within normal ranges in 50% to 60% of patients. Since the effects of pituitary irradiation may not become maximal for several years, adjunctive therapy with Octreotide acetate to reduce blood levels of growth hormone and IGF-I (somatomedin C) offers potential benefit before the effects of irradiation are manifested.
Improvement in clinical signs and symptoms or reduction in tumor size or rate of growth were not shown in clinical trials performed with Octreotide acetate; these trials were not optimally designed to detect such effects.
Carcinoid Tumors
Octreotide acetate is indicated for the symptomatic treatment of patients with metastatic carcinoid tumors where it suppresses or inhibits the severe diarrhea and flushing episodes associated with the disease.
Octreotide acetate studies were not designed to show an effect on the size, rate of growth or development of metastases.
Vasoactive Intestinal Peptide Tumors (VIPomas)
Octreotide acetate is indicated for the treatment of the profuse watery diarrhea associated with VIP-secreting tumors. Octreotide acetate studies were not designed to show an effect on the size, rate of growth or development of metastases.
• Injection 50 mcg/1ml: Box of 5Ampoules
[view] =>• Injection 50 mcg/1ml: Box of 5Ampoules
) ) [field_pdf] => Array ( [0] => Array ( [fid] => 234 [uid] => 1 [filename] => octreotide.pdf [filepath] => sites/default/files/pdf/octreotide.pdf [filemime] => application/pdf [filesize] => 350973 [status] => 1 [timestamp] => 1329503863 [list] => 1 [data] => [i18nsync] => 1 [nid] => 266 [view] => ) ) [field_pharmacokinetics] => Array ( [0] => Array ( [value] => After subcutaneous injection, Octreotide is absorbed rapidly and completely from the injection site. Peak concentrations of 5.2 ng/mL (100-mcg dose) were reached 0.4 hours after dosing. Using a specific radioimmunoassay, intravenous and subcutaneous doses were found to be bioequivalent. Peak concentrations and area under the curve values were dose proportional after intravenous single doses up to 200 mcg and subcutaneous single doses up to 500 mcg and after subcutaneous multiple doses up to 500 mcg t.i.d. (1500 mcg/day). In healthy volunteers the distribution of Octreotide from plasma was rapid (tα1/2=0.2 h), the volume of distribution (Vdss) was estimated to be 13.6 L, and the total body clearance ranged from 7 L/hr to 10 L/hr. In blood, the distribution into the erythrocytes was found to be negligible and about 65% was bound in the plasma in a concentration-independent manner. Binding was mainly to lipoprotein and, to a lesser extent, to albumin. The elimination of Octreotide from plasma had an apparent half-life of 1.7 to 1.9 hours compared with 1 to 3 minutes with the natural hormone. The duration of action of Octreotide acetate is variable but extends up to 12 hours depending upon the type of tumor. About 32% of the dose is excreted unchanged into the urine. In an elderly population, dose adjustments may be necessary due to a significant increase in the half-life (46%) and a significant decrease in the clearance (26%) of the drug. In patients with acromegaly, the pharmacokinetics differ somewhat from those in healthy volunteers. A mean peak concentration of 2.8 ng/mL (100-mcg dose) was reached in 0.7 hours after subcutaneous dosing. The volume of distribution (Vdss) was estimated to be 21.6 ± 8.5 L and the total body clearance was increased to 18 L/h. The mean percent of the drug bound was 41.2%. The disposition and elimination half-lives were similar to normals. In patients with renal impairment the elimination of Octreotide from plasma was prolonged and total body clearance reduced. In mild renal impairment (ClCR40 to 60 mL/min) Octreotide t1/2 was 2.4 hours and total body clearance was 8.8 L/hr, in moderate impairment (ClCR10 to 39 mL/min) t1/2 was 3.0 hours and total body clearance 7.3 L/hr, and in severely renally impaired patients not requiring dialysis (ClCR<10 mL/min) t1/2 was 3.1 hours and total body clearance was 7.6 L/hr. In patients with severe renal failure requiring dialysis, total body clearance was reduced to about half that found in healthy subjects (from approximately 10 L/hr to 4.5 L/hr). Patients with liver cirrhosis showed prolonged elimination of drug, with Octreotide t1/2 increasing to 3.7 hr and total body clearance decreasing to 5.9 L/hr, whereas patients with fatty liver disease showed t1/2 increased to 3.4 hr and total body clearance of 8.2 L/hr. [format] => 1 [safe] =>After subcutaneous injection, Octreotide is absorbed rapidly and completely from the injection site. Peak concentrations of 5.2 ng/mL (100-mcg dose) were reached 0.4 hours after dosing. Using a specific radioimmunoassay, intravenous and subcutaneous doses were found to be bioequivalent. Peak concentrations and area under the curve values were dose proportional after intravenous single doses up to 200 mcg and subcutaneous single doses up to 500 mcg and after subcutaneous multiple doses up to 500 mcg t.i.d. (1500 mcg/day).
In healthy volunteers the distribution of Octreotide from plasma was rapid (tα1/2=0.2 h), the volume of distribution (Vdss) was estimated to be 13.6 L, and the total body clearance ranged from 7 L/hr to 10 L/hr. In blood, the distribution into the erythrocytes was found to be negligible and about 65% was bound in the plasma in a concentration-independent manner. Binding was mainly to lipoprotein and, to a lesser extent, to albumin.
The elimination of Octreotide from plasma had an apparent half-life of 1.7 to 1.9 hours compared with 1 to 3 minutes with the natural hormone. The duration of action of Octreotide acetate is variable but extends up to 12 hours depending upon the type of tumor. About 32% of the dose is excreted unchanged into the urine. In an elderly population, dose adjustments may be necessary due to a significant increase in the half-life (46%) and a significant decrease in the clearance (26%) of the drug.
In patients with acromegaly, the pharmacokinetics differ somewhat from those in healthy volunteers. A mean peak concentration of 2.8 ng/mL (100-mcg dose) was reached in 0.7 hours after subcutaneous dosing. The volume of distribution (Vdss) was estimated to be 21.6 ± 8.5 L and the total body clearance was increased to 18 L/h. The mean percent of the drug bound was 41.2%. The disposition and elimination half-lives were similar to normals.
In patients with renal impairment the elimination of Octreotide from plasma was prolonged and total body clearance reduced. In mild renal impairment (ClCR40 to 60 mL/min) Octreotide t1/2 was 2.4 hours and total body clearance was 8.8 L/hr, in moderate impairment (ClCR10 to 39 mL/min) t1/2 was 3.0 hours and total body clearance 7.3 L/hr, and in severely renally impaired patients not requiring dialysis (ClCR<10 mL/min) t1/2 was 3.1 hours and total body clearance was 7.6 L/hr. In patients with severe renal failure requiring dialysis, total body clearance was reduced to about half that found in healthy subjects (from approximately 10 L/hr to 4.5 L/hr).
Patients with liver cirrhosis showed prolonged elimination of drug, with Octreotide t1/2 increasing to 3.7 hr and total body clearance decreasing to 5.9 L/hr, whereas patients with fatty liver disease showed t1/2 increased to 3.4 hr and total body clearance of 8.2 L/hr.
After subcutaneous injection, Octreotide is absorbed rapidly and completely from the injection site. Peak concentrations of 5.2 ng/mL (100-mcg dose) were reached 0.4 hours after dosing. Using a specific radioimmunoassay, intravenous and subcutaneous doses were found to be bioequivalent. Peak concentrations and area under the curve values were dose proportional after intravenous single doses up to 200 mcg and subcutaneous single doses up to 500 mcg and after subcutaneous multiple doses up to 500 mcg t.i.d. (1500 mcg/day).
In healthy volunteers the distribution of Octreotide from plasma was rapid (tα1/2=0.2 h), the volume of distribution (Vdss) was estimated to be 13.6 L, and the total body clearance ranged from 7 L/hr to 10 L/hr. In blood, the distribution into the erythrocytes was found to be negligible and about 65% was bound in the plasma in a concentration-independent manner. Binding was mainly to lipoprotein and, to a lesser extent, to albumin.
The elimination of Octreotide from plasma had an apparent half-life of 1.7 to 1.9 hours compared with 1 to 3 minutes with the natural hormone. The duration of action of Octreotide acetate is variable but extends up to 12 hours depending upon the type of tumor. About 32% of the dose is excreted unchanged into the urine. In an elderly population, dose adjustments may be necessary due to a significant increase in the half-life (46%) and a significant decrease in the clearance (26%) of the drug.
In patients with acromegaly, the pharmacokinetics differ somewhat from those in healthy volunteers. A mean peak concentration of 2.8 ng/mL (100-mcg dose) was reached in 0.7 hours after subcutaneous dosing. The volume of distribution (Vdss) was estimated to be 21.6 ± 8.5 L and the total body clearance was increased to 18 L/h. The mean percent of the drug bound was 41.2%. The disposition and elimination half-lives were similar to normals.
In patients with renal impairment the elimination of Octreotide from plasma was prolonged and total body clearance reduced. In mild renal impairment (ClCR40 to 60 mL/min) Octreotide t1/2 was 2.4 hours and total body clearance was 8.8 L/hr, in moderate impairment (ClCR10 to 39 mL/min) t1/2 was 3.0 hours and total body clearance 7.3 L/hr, and in severely renally impaired patients not requiring dialysis (ClCR<10 mL/min) t1/2 was 3.1 hours and total body clearance was 7.6 L/hr. In patients with severe renal failure requiring dialysis, total body clearance was reduced to about half that found in healthy subjects (from approximately 10 L/hr to 4.5 L/hr).
Patients with liver cirrhosis showed prolonged elimination of drug, with Octreotide t1/2 increasing to 3.7 hr and total body clearance decreasing to 5.9 L/hr, whereas patients with fatty liver disease showed t1/2 increased to 3.4 hr and total body clearance of 8.2 L/hr.
Pituitary Hormones
[view] =>Pituitary Hormones
) ) [field_precautions] => Array ( [0] => Array ( [value] => Octreotide acetate alters the balance between the counter-regulatory hormones, insulin, glucagon and growth hormone, which may result in hypoglycemia or hyperglycemia. Octreotide acetate also suppresses secretion of thyroid stimulating hormone, which may result in hypothyroidism. Cardiac conduction abnormalities have also occurred during treatment with Octreotide acetate. However, the incidence of these adverse events during long-term therapy was determined vigorously only in acromegaly patients who, due to their underlying disease and/or the subsequent treatment they receive, are at an increased risk for the development of diabetes mellitus, hypothyroidism, and cardiovascular disease. Although the degree to which these abnormalities are related to Octreotide acetate therapy is not clear, new abnormalities of glycemic control, thyroid function and ECG developed during Octreotide acetate therapy as described below. [format] => 1 [safe] =>Octreotide acetate alters the balance between the counter-regulatory hormones, insulin, glucagon and growth hormone, which may result in hypoglycemia or hyperglycemia. Octreotide acetate also suppresses secretion of thyroid stimulating hormone, which may result in hypothyroidism. Cardiac conduction abnormalities have also occurred during treatment with Octreotide acetate. However, the incidence of these adverse events during long-term therapy was determined vigorously only in acromegaly patients who, due to their underlying disease and/or the subsequent treatment they receive, are at an increased risk for the development of diabetes mellitus, hypothyroidism, and cardiovascular disease. Although the degree to which these abnormalities are related to Octreotide acetate therapy is not clear, new abnormalities of glycemic control, thyroid function and ECG developed during Octreotide acetate therapy as described below.
[view] =>Octreotide acetate alters the balance between the counter-regulatory hormones, insulin, glucagon and growth hormone, which may result in hypoglycemia or hyperglycemia. Octreotide acetate also suppresses secretion of thyroid stimulating hormone, which may result in hypothyroidism. Cardiac conduction abnormalities have also occurred during treatment with Octreotide acetate. However, the incidence of these adverse events during long-term therapy was determined vigorously only in acromegaly patients who, due to their underlying disease and/or the subsequent treatment they receive, are at an increased risk for the development of diabetes mellitus, hypothyroidism, and cardiovascular disease. Although the degree to which these abnormalities are related to Octreotide acetate therapy is not clear, new abnormalities of glycemic control, thyroid function and ECG developed during Octreotide acetate therapy as described below.
) ) [field_pregnancy_category] => Array ( [0] => Array ( [value] => Category B [format] => 1 [safe] =>Category B
[view] =>Category B
) ) [field_references] => Array ( [0] => Array ( [value] => [format] => [safe] => [view] => ) ) [field_side_effects] => Array ( [0] => Array ( [value] =>Gallbladder Abnormalities
Gallbladder abnormalities, especially stones and/or biliary sludge, frequently develop in patients on chronic Octreotide acetate therapy .
Cardiac
In acromegalics, sinus bradycardia (<50 bpm) developed in 25%; conduction abnormalities occurred in 10% and arrhythmias developed in 9% of patients during Octreotide acetate therapy.
Gastrointestinal
Diarrhea, loose stools, nausea and abdominal discomfort were each seen in 34% to 61% of acromegalic patients in U.S. studies although only 2.6% of the patients discontinued therapy due to these symptoms. These symptoms were seen in 5% to 10% of patients with other disorders.
The frequency of these symptoms was not dose-related, but diarrhea and abdominal discomfort generally resolved more quickly in patients treated with 300 mcg/day than in those treated with 750 mcg/day. Vomiting, flatulence, abnormal stools, abdominal distention, and constipation were each seen in less than 10% of patients.
In rare instances, gastrointestinal side effects may resemble acute intestinal obstruction, with progressive abdominal distension, severe epigastric pain, abdominal tenderness and guarding.
Hypo/Hyperglycemia
Hypoglycemia and hyperglycemia occurred in 3% and 16% of acromegalic patients, respectively, but only in about 1.5% of other patients. Symptoms of hypoglycemia were noted in approximately 2% of patients.
Hypothyroidism
In acromegalics, biochemical hypothyroidism alone occurred in 12% while goiter occurred in 6% during Octreotide acetate therapy. In patients without acromegaly, hypothyroidism has only been reported in several isolated patients and goiter has not been reported.
Other Adverse Events
Pain on injection was reported in 7.7%, headache in 6% and dizziness in 5%. Pancreatitis was also observed.
Gallbladder Abnormalities
Gallbladder abnormalities, especially stones and/or biliary sludge, frequently develop in patients on chronic Octreotide acetate therapy .
Cardiac
In acromegalics, sinus bradycardia (<50 bpm) developed in 25%; conduction abnormalities occurred in 10% and arrhythmias developed in 9% of patients during Octreotide acetate therapy.
Gastrointestinal
Diarrhea, loose stools, nausea and abdominal discomfort were each seen in 34% to 61% of acromegalic patients in U.S. studies although only 2.6% of the patients discontinued therapy due to these symptoms. These symptoms were seen in 5% to 10% of patients with other disorders.
The frequency of these symptoms was not dose-related, but diarrhea and abdominal discomfort generally resolved more quickly in patients treated with 300 mcg/day than in those treated with 750 mcg/day. Vomiting, flatulence, abnormal stools, abdominal distention, and constipation were each seen in less than 10% of patients.
In rare instances, gastrointestinal side effects may resemble acute intestinal obstruction, with progressive abdominal distension, severe epigastric pain, abdominal tenderness and guarding.
Hypo/Hyperglycemia
Hypoglycemia and hyperglycemia occurred in 3% and 16% of acromegalic patients, respectively, but only in about 1.5% of other patients. Symptoms of hypoglycemia were noted in approximately 2% of patients.
Hypothyroidism
In acromegalics, biochemical hypothyroidism alone occurred in 12% while goiter occurred in 6% during Octreotide acetate therapy. In patients without acromegaly, hypothyroidism has only been reported in several isolated patients and goiter has not been reported.
Other Adverse Events
Pain on injection was reported in 7.7%, headache in 6% and dizziness in 5%. Pancreatitis was also observed.
Gallbladder Abnormalities
Gallbladder abnormalities, especially stones and/or biliary sludge, frequently develop in patients on chronic Octreotide acetate therapy .
Cardiac
In acromegalics, sinus bradycardia (<50 bpm) developed in 25%; conduction abnormalities occurred in 10% and arrhythmias developed in 9% of patients during Octreotide acetate therapy.
Gastrointestinal
Diarrhea, loose stools, nausea and abdominal discomfort were each seen in 34% to 61% of acromegalic patients in U.S. studies although only 2.6% of the patients discontinued therapy due to these symptoms. These symptoms were seen in 5% to 10% of patients with other disorders.
The frequency of these symptoms was not dose-related, but diarrhea and abdominal discomfort generally resolved more quickly in patients treated with 300 mcg/day than in those treated with 750 mcg/day. Vomiting, flatulence, abnormal stools, abdominal distention, and constipation were each seen in less than 10% of patients.
In rare instances, gastrointestinal side effects may resemble acute intestinal obstruction, with progressive abdominal distension, severe epigastric pain, abdominal tenderness and guarding.
Hypo/Hyperglycemia
Hypoglycemia and hyperglycemia occurred in 3% and 16% of acromegalic patients, respectively, but only in about 1.5% of other patients. Symptoms of hypoglycemia were noted in approximately 2% of patients.
Hypothyroidism
In acromegalics, biochemical hypothyroidism alone occurred in 12% while goiter occurred in 6% during Octreotide acetate therapy. In patients without acromegaly, hypothyroidism has only been reported in several isolated patients and goiter has not been reported.
Other Adverse Events
Pain on injection was reported in 7.7%, headache in 6% and dizziness in 5%. Pancreatitis was also observed.
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
Somatostatin Analogue
[view] =>Somatostatin Analogue
) ) [field_related_products] => Array ( [0] => Array ( [nid] => [i18nsync] => 1 [safe] => Array ( ) [view] => ) [1] => Array ( [nid] => [i18nsync] => 1 [safe] => Array ( ) [view] => ) [2] => Array ( [nid] => [i18nsync] => 1 [safe] => Array ( ) [view] => ) ) [taxonomy] => Array ( [5] => stdClass Object ( [tid] => 5 [vid] => 1 [name] => Hormonal Drugs [description] => [weight] => 3 [language] => [trid] => 0 [v_weight_unused] => 0 ) ) [build_mode] => 0 [readmore] => [content] => Array ( [field_one_image] => Array ( [#type_name] => product [#context] => full [#field_name] => field_one_image [#post_render] => Array ( [0] => content_field_wrapper_post_render ) [#weight] => -3 [field] => Array ( [#description] => [items] => Array ( [0] => Array ( [#formatter] => image_plain [#node] => stdClass Object *RECURSION* [#type_name] => product [#field_name] => field_one_image [#weight] => 0 [#theme] => imagefield_formatter_image_plain [#item] => Array ( [fid] => 5977 [uid] => 2 [filename] => jbh_ampwl_khtwsttyn.jpg [filepath] => sites/default/files/images/jbh_ampwl_khtwsttyn.jpg [filemime] => image/jpeg [filesize] => 163513 [status] => 1 [timestamp] => 1657967205 [list] => 1 [data] => Array ( [alt] => [title] => ) [i18nsync] => 1 [nid] => 266 [#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] => )
[#title] =>
[#description] =>
[#children] =>
)
[#title] =>
[#description] =>
[#children] =>  [#printed] => 1
)
[#single] => 1
[#attributes] => Array
(
)
[#required] =>
[#parents] => Array
(
)
[#tree] =>
[#context] => full
[#page] => 1
[#field_name] => field_one_image
[#title] => Image
[#access] => 1
[#label_display] => above
[#teaser] =>
[#node] => stdClass Object
*RECURSION*
[#type] => content_field
[#children] =>
[#printed] => 1
)
[#single] => 1
[#attributes] => Array
(
)
[#required] =>
[#parents] => Array
(
)
[#tree] =>
[#context] => full
[#page] => 1
[#field_name] => field_one_image
[#title] => Image
[#access] => 1
[#label_display] => above
[#teaser] =>
[#node] => stdClass Object
*RECURSION*
[#type] => content_field
[#children] =>  [#printed] => 1
)
[#title] =>
[#description] =>
[#children] =>
[#printed] => 1
)
[#title] =>
[#description] =>
[#children] => 
OCTOSTATIN®
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>OCTOSTATIN®
) [#title] => [#description] => [#children] =>OCTOSTATIN®
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_brand_name [#title] => Brand Name [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>OCTOSTATIN®
[#printed] => 1 ) [#title] => [#description] => [#children] =>OCTOSTATIN®
Injection 50 mcg/1ml
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Injection 50 mcg/1ml
) [#title] => [#description] => [#children] =>Injection 50 mcg/1ml
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_dosage_form [#title] => Dosage Form [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Injection 50 mcg/1ml
[#printed] => 1 ) [#title] => [#description] => [#children] =>Injection 50 mcg/1ml
Pituitary Hormones
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Pituitary Hormones
) [#title] => [#description] => [#children] =>Pituitary Hormones
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_pharmacological_category [#title] => Pharmacological Category [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Pituitary Hormones
[#printed] => 1 ) [#title] => [#description] => [#children] =>Pituitary Hormones
Somatostatin Analogue
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Somatostatin Analogue
) [#title] => [#description] => [#children] =>Somatostatin Analogue
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_therapeutic_category [#title] => Therapeutic Category [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Somatostatin Analogue
[#printed] => 1 ) [#title] => [#description] => [#children] =>Somatostatin Analogue
Category B
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Category B
) [#title] => [#description] => [#children] =>Category B
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_pregnancy_category [#title] => Pregnancy Category [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Category B
[#printed] => 1 ) [#title] => [#description] => [#children] =>Category B
Octreotide acetate exerts pharmacologic actions similar to the natural hormone, somatostatin. It is an even more potent inhibitor of growth hormone, glucagon, and insulin than somatostatin. Like somatostatin, it also suppresses LH response to GnRH, decreases splanchnic blood flow, and inhibits release of serotonin, gastrin, vasoactive intestinal peptide, secretin, motilin, and pancreatic polypeptide.
[#title] => [#description] => [#printed] => 1 ) [field_pharmacokinetics] => Array ( [#type_name] => product [#context] => full [#field_name] => field_pharmacokinetics [#post_render] => Array ( [0] => content_field_wrapper_post_render ) [#weight] => 4 [field] => Array ( [#description] => [items] => Array ( [0] => Array ( [#formatter] => default [#node] => stdClass Object *RECURSION* [#type_name] => product [#field_name] => field_pharmacokinetics [#weight] => 0 [#theme] => text_formatter_default [#item] => Array ( [value] => After subcutaneous injection, Octreotide is absorbed rapidly and completely from the injection site. Peak concentrations of 5.2 ng/mL (100-mcg dose) were reached 0.4 hours after dosing. Using a specific radioimmunoassay, intravenous and subcutaneous doses were found to be bioequivalent. Peak concentrations and area under the curve values were dose proportional after intravenous single doses up to 200 mcg and subcutaneous single doses up to 500 mcg and after subcutaneous multiple doses up to 500 mcg t.i.d. (1500 mcg/day). In healthy volunteers the distribution of Octreotide from plasma was rapid (tα1/2=0.2 h), the volume of distribution (Vdss) was estimated to be 13.6 L, and the total body clearance ranged from 7 L/hr to 10 L/hr. In blood, the distribution into the erythrocytes was found to be negligible and about 65% was bound in the plasma in a concentration-independent manner. Binding was mainly to lipoprotein and, to a lesser extent, to albumin. The elimination of Octreotide from plasma had an apparent half-life of 1.7 to 1.9 hours compared with 1 to 3 minutes with the natural hormone. The duration of action of Octreotide acetate is variable but extends up to 12 hours depending upon the type of tumor. About 32% of the dose is excreted unchanged into the urine. In an elderly population, dose adjustments may be necessary due to a significant increase in the half-life (46%) and a significant decrease in the clearance (26%) of the drug. In patients with acromegaly, the pharmacokinetics differ somewhat from those in healthy volunteers. A mean peak concentration of 2.8 ng/mL (100-mcg dose) was reached in 0.7 hours after subcutaneous dosing. The volume of distribution (Vdss) was estimated to be 21.6 ± 8.5 L and the total body clearance was increased to 18 L/h. The mean percent of the drug bound was 41.2%. The disposition and elimination half-lives were similar to normals. In patients with renal impairment the elimination of Octreotide from plasma was prolonged and total body clearance reduced. In mild renal impairment (ClCR40 to 60 mL/min) Octreotide t1/2 was 2.4 hours and total body clearance was 8.8 L/hr, in moderate impairment (ClCR10 to 39 mL/min) t1/2 was 3.0 hours and total body clearance 7.3 L/hr, and in severely renally impaired patients not requiring dialysis (ClCR<10 mL/min) t1/2 was 3.1 hours and total body clearance was 7.6 L/hr. In patients with severe renal failure requiring dialysis, total body clearance was reduced to about half that found in healthy subjects (from approximately 10 L/hr to 4.5 L/hr). Patients with liver cirrhosis showed prolonged elimination of drug, with Octreotide t1/2 increasing to 3.7 hr and total body clearance decreasing to 5.9 L/hr, whereas patients with fatty liver disease showed t1/2 increased to 3.4 hr and total body clearance of 8.2 L/hr. [format] => 1 [safe] =>After subcutaneous injection, Octreotide is absorbed rapidly and completely from the injection site. Peak concentrations of 5.2 ng/mL (100-mcg dose) were reached 0.4 hours after dosing. Using a specific radioimmunoassay, intravenous and subcutaneous doses were found to be bioequivalent. Peak concentrations and area under the curve values were dose proportional after intravenous single doses up to 200 mcg and subcutaneous single doses up to 500 mcg and after subcutaneous multiple doses up to 500 mcg t.i.d. (1500 mcg/day).
In healthy volunteers the distribution of Octreotide from plasma was rapid (tα1/2=0.2 h), the volume of distribution (Vdss) was estimated to be 13.6 L, and the total body clearance ranged from 7 L/hr to 10 L/hr. In blood, the distribution into the erythrocytes was found to be negligible and about 65% was bound in the plasma in a concentration-independent manner. Binding was mainly to lipoprotein and, to a lesser extent, to albumin.
The elimination of Octreotide from plasma had an apparent half-life of 1.7 to 1.9 hours compared with 1 to 3 minutes with the natural hormone. The duration of action of Octreotide acetate is variable but extends up to 12 hours depending upon the type of tumor. About 32% of the dose is excreted unchanged into the urine. In an elderly population, dose adjustments may be necessary due to a significant increase in the half-life (46%) and a significant decrease in the clearance (26%) of the drug.
In patients with acromegaly, the pharmacokinetics differ somewhat from those in healthy volunteers. A mean peak concentration of 2.8 ng/mL (100-mcg dose) was reached in 0.7 hours after subcutaneous dosing. The volume of distribution (Vdss) was estimated to be 21.6 ± 8.5 L and the total body clearance was increased to 18 L/h. The mean percent of the drug bound was 41.2%. The disposition and elimination half-lives were similar to normals.
In patients with renal impairment the elimination of Octreotide from plasma was prolonged and total body clearance reduced. In mild renal impairment (ClCR40 to 60 mL/min) Octreotide t1/2 was 2.4 hours and total body clearance was 8.8 L/hr, in moderate impairment (ClCR10 to 39 mL/min) t1/2 was 3.0 hours and total body clearance 7.3 L/hr, and in severely renally impaired patients not requiring dialysis (ClCR<10 mL/min) t1/2 was 3.1 hours and total body clearance was 7.6 L/hr. In patients with severe renal failure requiring dialysis, total body clearance was reduced to about half that found in healthy subjects (from approximately 10 L/hr to 4.5 L/hr).
Patients with liver cirrhosis showed prolonged elimination of drug, with Octreotide t1/2 increasing to 3.7 hr and total body clearance decreasing to 5.9 L/hr, whereas patients with fatty liver disease showed t1/2 increased to 3.4 hr and total body clearance of 8.2 L/hr.
After subcutaneous injection, Octreotide is absorbed rapidly and completely from the injection site. Peak concentrations of 5.2 ng/mL (100-mcg dose) were reached 0.4 hours after dosing. Using a specific radioimmunoassay, intravenous and subcutaneous doses were found to be bioequivalent. Peak concentrations and area under the curve values were dose proportional after intravenous single doses up to 200 mcg and subcutaneous single doses up to 500 mcg and after subcutaneous multiple doses up to 500 mcg t.i.d. (1500 mcg/day).
In healthy volunteers the distribution of Octreotide from plasma was rapid (tα1/2=0.2 h), the volume of distribution (Vdss) was estimated to be 13.6 L, and the total body clearance ranged from 7 L/hr to 10 L/hr. In blood, the distribution into the erythrocytes was found to be negligible and about 65% was bound in the plasma in a concentration-independent manner. Binding was mainly to lipoprotein and, to a lesser extent, to albumin.
The elimination of Octreotide from plasma had an apparent half-life of 1.7 to 1.9 hours compared with 1 to 3 minutes with the natural hormone. The duration of action of Octreotide acetate is variable but extends up to 12 hours depending upon the type of tumor. About 32% of the dose is excreted unchanged into the urine. In an elderly population, dose adjustments may be necessary due to a significant increase in the half-life (46%) and a significant decrease in the clearance (26%) of the drug.
In patients with acromegaly, the pharmacokinetics differ somewhat from those in healthy volunteers. A mean peak concentration of 2.8 ng/mL (100-mcg dose) was reached in 0.7 hours after subcutaneous dosing. The volume of distribution (Vdss) was estimated to be 21.6 ± 8.5 L and the total body clearance was increased to 18 L/h. The mean percent of the drug bound was 41.2%. The disposition and elimination half-lives were similar to normals.
In patients with renal impairment the elimination of Octreotide from plasma was prolonged and total body clearance reduced. In mild renal impairment (ClCR40 to 60 mL/min) Octreotide t1/2 was 2.4 hours and total body clearance was 8.8 L/hr, in moderate impairment (ClCR10 to 39 mL/min) t1/2 was 3.0 hours and total body clearance 7.3 L/hr, and in severely renally impaired patients not requiring dialysis (ClCR<10 mL/min) t1/2 was 3.1 hours and total body clearance was 7.6 L/hr. In patients with severe renal failure requiring dialysis, total body clearance was reduced to about half that found in healthy subjects (from approximately 10 L/hr to 4.5 L/hr).
Patients with liver cirrhosis showed prolonged elimination of drug, with Octreotide t1/2 increasing to 3.7 hr and total body clearance decreasing to 5.9 L/hr, whereas patients with fatty liver disease showed t1/2 increased to 3.4 hr and total body clearance of 8.2 L/hr.
After subcutaneous injection, Octreotide is absorbed rapidly and completely from the injection site. Peak concentrations of 5.2 ng/mL (100-mcg dose) were reached 0.4 hours after dosing. Using a specific radioimmunoassay, intravenous and subcutaneous doses were found to be bioequivalent. Peak concentrations and area under the curve values were dose proportional after intravenous single doses up to 200 mcg and subcutaneous single doses up to 500 mcg and after subcutaneous multiple doses up to 500 mcg t.i.d. (1500 mcg/day).
In healthy volunteers the distribution of Octreotide from plasma was rapid (tα1/2=0.2 h), the volume of distribution (Vdss) was estimated to be 13.6 L, and the total body clearance ranged from 7 L/hr to 10 L/hr. In blood, the distribution into the erythrocytes was found to be negligible and about 65% was bound in the plasma in a concentration-independent manner. Binding was mainly to lipoprotein and, to a lesser extent, to albumin.
The elimination of Octreotide from plasma had an apparent half-life of 1.7 to 1.9 hours compared with 1 to 3 minutes with the natural hormone. The duration of action of Octreotide acetate is variable but extends up to 12 hours depending upon the type of tumor. About 32% of the dose is excreted unchanged into the urine. In an elderly population, dose adjustments may be necessary due to a significant increase in the half-life (46%) and a significant decrease in the clearance (26%) of the drug.
In patients with acromegaly, the pharmacokinetics differ somewhat from those in healthy volunteers. A mean peak concentration of 2.8 ng/mL (100-mcg dose) was reached in 0.7 hours after subcutaneous dosing. The volume of distribution (Vdss) was estimated to be 21.6 ± 8.5 L and the total body clearance was increased to 18 L/h. The mean percent of the drug bound was 41.2%. The disposition and elimination half-lives were similar to normals.
In patients with renal impairment the elimination of Octreotide from plasma was prolonged and total body clearance reduced. In mild renal impairment (ClCR40 to 60 mL/min) Octreotide t1/2 was 2.4 hours and total body clearance was 8.8 L/hr, in moderate impairment (ClCR10 to 39 mL/min) t1/2 was 3.0 hours and total body clearance 7.3 L/hr, and in severely renally impaired patients not requiring dialysis (ClCR<10 mL/min) t1/2 was 3.1 hours and total body clearance was 7.6 L/hr. In patients with severe renal failure requiring dialysis, total body clearance was reduced to about half that found in healthy subjects (from approximately 10 L/hr to 4.5 L/hr).
Patients with liver cirrhosis showed prolonged elimination of drug, with Octreotide t1/2 increasing to 3.7 hr and total body clearance decreasing to 5.9 L/hr, whereas patients with fatty liver disease showed t1/2 increased to 3.4 hr and total body clearance of 8.2 L/hr.
After subcutaneous injection, Octreotide is absorbed rapidly and completely from the injection site. Peak concentrations of 5.2 ng/mL (100-mcg dose) were reached 0.4 hours after dosing. Using a specific radioimmunoassay, intravenous and subcutaneous doses were found to be bioequivalent. Peak concentrations and area under the curve values were dose proportional after intravenous single doses up to 200 mcg and subcutaneous single doses up to 500 mcg and after subcutaneous multiple doses up to 500 mcg t.i.d. (1500 mcg/day).
In healthy volunteers the distribution of Octreotide from plasma was rapid (tα1/2=0.2 h), the volume of distribution (Vdss) was estimated to be 13.6 L, and the total body clearance ranged from 7 L/hr to 10 L/hr. In blood, the distribution into the erythrocytes was found to be negligible and about 65% was bound in the plasma in a concentration-independent manner. Binding was mainly to lipoprotein and, to a lesser extent, to albumin.
The elimination of Octreotide from plasma had an apparent half-life of 1.7 to 1.9 hours compared with 1 to 3 minutes with the natural hormone. The duration of action of Octreotide acetate is variable but extends up to 12 hours depending upon the type of tumor. About 32% of the dose is excreted unchanged into the urine. In an elderly population, dose adjustments may be necessary due to a significant increase in the half-life (46%) and a significant decrease in the clearance (26%) of the drug.
In patients with acromegaly, the pharmacokinetics differ somewhat from those in healthy volunteers. A mean peak concentration of 2.8 ng/mL (100-mcg dose) was reached in 0.7 hours after subcutaneous dosing. The volume of distribution (Vdss) was estimated to be 21.6 ± 8.5 L and the total body clearance was increased to 18 L/h. The mean percent of the drug bound was 41.2%. The disposition and elimination half-lives were similar to normals.
In patients with renal impairment the elimination of Octreotide from plasma was prolonged and total body clearance reduced. In mild renal impairment (ClCR40 to 60 mL/min) Octreotide t1/2 was 2.4 hours and total body clearance was 8.8 L/hr, in moderate impairment (ClCR10 to 39 mL/min) t1/2 was 3.0 hours and total body clearance 7.3 L/hr, and in severely renally impaired patients not requiring dialysis (ClCR<10 mL/min) t1/2 was 3.1 hours and total body clearance was 7.6 L/hr. In patients with severe renal failure requiring dialysis, total body clearance was reduced to about half that found in healthy subjects (from approximately 10 L/hr to 4.5 L/hr).
Patients with liver cirrhosis showed prolonged elimination of drug, with Octreotide t1/2 increasing to 3.7 hr and total body clearance decreasing to 5.9 L/hr, whereas patients with fatty liver disease showed t1/2 increased to 3.4 hr and total body clearance of 8.2 L/hr.
After subcutaneous injection, Octreotide is absorbed rapidly and completely from the injection site. Peak concentrations of 5.2 ng/mL (100-mcg dose) were reached 0.4 hours after dosing. Using a specific radioimmunoassay, intravenous and subcutaneous doses were found to be bioequivalent. Peak concentrations and area under the curve values were dose proportional after intravenous single doses up to 200 mcg and subcutaneous single doses up to 500 mcg and after subcutaneous multiple doses up to 500 mcg t.i.d. (1500 mcg/day).
In healthy volunteers the distribution of Octreotide from plasma was rapid (tα1/2=0.2 h), the volume of distribution (Vdss) was estimated to be 13.6 L, and the total body clearance ranged from 7 L/hr to 10 L/hr. In blood, the distribution into the erythrocytes was found to be negligible and about 65% was bound in the plasma in a concentration-independent manner. Binding was mainly to lipoprotein and, to a lesser extent, to albumin.
The elimination of Octreotide from plasma had an apparent half-life of 1.7 to 1.9 hours compared with 1 to 3 minutes with the natural hormone. The duration of action of Octreotide acetate is variable but extends up to 12 hours depending upon the type of tumor. About 32% of the dose is excreted unchanged into the urine. In an elderly population, dose adjustments may be necessary due to a significant increase in the half-life (46%) and a significant decrease in the clearance (26%) of the drug.
In patients with acromegaly, the pharmacokinetics differ somewhat from those in healthy volunteers. A mean peak concentration of 2.8 ng/mL (100-mcg dose) was reached in 0.7 hours after subcutaneous dosing. The volume of distribution (Vdss) was estimated to be 21.6 ± 8.5 L and the total body clearance was increased to 18 L/h. The mean percent of the drug bound was 41.2%. The disposition and elimination half-lives were similar to normals.
In patients with renal impairment the elimination of Octreotide from plasma was prolonged and total body clearance reduced. In mild renal impairment (ClCR40 to 60 mL/min) Octreotide t1/2 was 2.4 hours and total body clearance was 8.8 L/hr, in moderate impairment (ClCR10 to 39 mL/min) t1/2 was 3.0 hours and total body clearance 7.3 L/hr, and in severely renally impaired patients not requiring dialysis (ClCR<10 mL/min) t1/2 was 3.1 hours and total body clearance was 7.6 L/hr. In patients with severe renal failure requiring dialysis, total body clearance was reduced to about half that found in healthy subjects (from approximately 10 L/hr to 4.5 L/hr).
Patients with liver cirrhosis showed prolonged elimination of drug, with Octreotide t1/2 increasing to 3.7 hr and total body clearance decreasing to 5.9 L/hr, whereas patients with fatty liver disease showed t1/2 increased to 3.4 hr and total body clearance of 8.2 L/hr.
Acromegaly
Octreotide acetate is indicated to reduce blood levels of growth hormone and IGF-I (somatomedin C) in acromegaly patients who have had inadequate response to or cannot be treated with surgical resection, pituitary irradiation, and bromocriptine mesylate at maximally tolerated doses. The goal is to achieve normalization of growth hormone and IGF-I (somatomedin C) levels. In patients with acromegaly, Octreotide acetate reduces growth hormone to within normal ranges in 50% of patients and reduces IGF-I (somatomedin C) to within normal ranges in 50% to 60% of patients. Since the effects of pituitary irradiation may not become maximal for several years, adjunctive therapy with Octreotide acetate to reduce blood levels of growth hormone and IGF-I (somatomedin C) offers potential benefit before the effects of irradiation are manifested.
Improvement in clinical signs and symptoms or reduction in tumor size or rate of growth were not shown in clinical trials performed with Octreotide acetate; these trials were not optimally designed to detect such effects.
Carcinoid Tumors
Octreotide acetate is indicated for the symptomatic treatment of patients with metastatic carcinoid tumors where it suppresses or inhibits the severe diarrhea and flushing episodes associated with the disease.
Octreotide acetate studies were not designed to show an effect on the size, rate of growth or development of metastases.
Vasoactive Intestinal Peptide Tumors (VIPomas)
Octreotide acetate is indicated for the treatment of the profuse watery diarrhea associated with VIP-secreting tumors. Octreotide acetate studies were not designed to show an effect on the size, rate of growth or development of metastases.
Acromegaly
Octreotide acetate is indicated to reduce blood levels of growth hormone and IGF-I (somatomedin C) in acromegaly patients who have had inadequate response to or cannot be treated with surgical resection, pituitary irradiation, and bromocriptine mesylate at maximally tolerated doses. The goal is to achieve normalization of growth hormone and IGF-I (somatomedin C) levels. In patients with acromegaly, Octreotide acetate reduces growth hormone to within normal ranges in 50% of patients and reduces IGF-I (somatomedin C) to within normal ranges in 50% to 60% of patients. Since the effects of pituitary irradiation may not become maximal for several years, adjunctive therapy with Octreotide acetate to reduce blood levels of growth hormone and IGF-I (somatomedin C) offers potential benefit before the effects of irradiation are manifested.
Improvement in clinical signs and symptoms or reduction in tumor size or rate of growth were not shown in clinical trials performed with Octreotide acetate; these trials were not optimally designed to detect such effects.
Carcinoid Tumors
Octreotide acetate is indicated for the symptomatic treatment of patients with metastatic carcinoid tumors where it suppresses or inhibits the severe diarrhea and flushing episodes associated with the disease.
Octreotide acetate studies were not designed to show an effect on the size, rate of growth or development of metastases.
Vasoactive Intestinal Peptide Tumors (VIPomas)
Octreotide acetate is indicated for the treatment of the profuse watery diarrhea associated with VIP-secreting tumors. Octreotide acetate studies were not designed to show an effect on the size, rate of growth or development of metastases.
Acromegaly
Octreotide acetate is indicated to reduce blood levels of growth hormone and IGF-I (somatomedin C) in acromegaly patients who have had inadequate response to or cannot be treated with surgical resection, pituitary irradiation, and bromocriptine mesylate at maximally tolerated doses. The goal is to achieve normalization of growth hormone and IGF-I (somatomedin C) levels. In patients with acromegaly, Octreotide acetate reduces growth hormone to within normal ranges in 50% of patients and reduces IGF-I (somatomedin C) to within normal ranges in 50% to 60% of patients. Since the effects of pituitary irradiation may not become maximal for several years, adjunctive therapy with Octreotide acetate to reduce blood levels of growth hormone and IGF-I (somatomedin C) offers potential benefit before the effects of irradiation are manifested.
Improvement in clinical signs and symptoms or reduction in tumor size or rate of growth were not shown in clinical trials performed with Octreotide acetate; these trials were not optimally designed to detect such effects.
Carcinoid Tumors
Octreotide acetate is indicated for the symptomatic treatment of patients with metastatic carcinoid tumors where it suppresses or inhibits the severe diarrhea and flushing episodes associated with the disease.
Octreotide acetate studies were not designed to show an effect on the size, rate of growth or development of metastases.
Vasoactive Intestinal Peptide Tumors (VIPomas)
Octreotide acetate is indicated for the treatment of the profuse watery diarrhea associated with VIP-secreting tumors. Octreotide acetate studies were not designed to show an effect on the size, rate of growth or development of metastases.
Acromegaly
Octreotide acetate is indicated to reduce blood levels of growth hormone and IGF-I (somatomedin C) in acromegaly patients who have had inadequate response to or cannot be treated with surgical resection, pituitary irradiation, and bromocriptine mesylate at maximally tolerated doses. The goal is to achieve normalization of growth hormone and IGF-I (somatomedin C) levels. In patients with acromegaly, Octreotide acetate reduces growth hormone to within normal ranges in 50% of patients and reduces IGF-I (somatomedin C) to within normal ranges in 50% to 60% of patients. Since the effects of pituitary irradiation may not become maximal for several years, adjunctive therapy with Octreotide acetate to reduce blood levels of growth hormone and IGF-I (somatomedin C) offers potential benefit before the effects of irradiation are manifested.
Improvement in clinical signs and symptoms or reduction in tumor size or rate of growth were not shown in clinical trials performed with Octreotide acetate; these trials were not optimally designed to detect such effects.
Carcinoid Tumors
Octreotide acetate is indicated for the symptomatic treatment of patients with metastatic carcinoid tumors where it suppresses or inhibits the severe diarrhea and flushing episodes associated with the disease.
Octreotide acetate studies were not designed to show an effect on the size, rate of growth or development of metastases.
Vasoactive Intestinal Peptide Tumors (VIPomas)
Octreotide acetate is indicated for the treatment of the profuse watery diarrhea associated with VIP-secreting tumors. Octreotide acetate studies were not designed to show an effect on the size, rate of growth or development of metastases.
Acromegaly
Octreotide acetate is indicated to reduce blood levels of growth hormone and IGF-I (somatomedin C) in acromegaly patients who have had inadequate response to or cannot be treated with surgical resection, pituitary irradiation, and bromocriptine mesylate at maximally tolerated doses. The goal is to achieve normalization of growth hormone and IGF-I (somatomedin C) levels. In patients with acromegaly, Octreotide acetate reduces growth hormone to within normal ranges in 50% of patients and reduces IGF-I (somatomedin C) to within normal ranges in 50% to 60% of patients. Since the effects of pituitary irradiation may not become maximal for several years, adjunctive therapy with Octreotide acetate to reduce blood levels of growth hormone and IGF-I (somatomedin C) offers potential benefit before the effects of irradiation are manifested.
Improvement in clinical signs and symptoms or reduction in tumor size or rate of growth were not shown in clinical trials performed with Octreotide acetate; these trials were not optimally designed to detect such effects.
Carcinoid Tumors
Octreotide acetate is indicated for the symptomatic treatment of patients with metastatic carcinoid tumors where it suppresses or inhibits the severe diarrhea and flushing episodes associated with the disease.
Octreotide acetate studies were not designed to show an effect on the size, rate of growth or development of metastases.
Vasoactive Intestinal Peptide Tumors (VIPomas)
Octreotide acetate is indicated for the treatment of the profuse watery diarrhea associated with VIP-secreting tumors. Octreotide acetate studies were not designed to show an effect on the size, rate of growth or development of metastases.
Acromegaly
Octreotide acetate is indicated to reduce blood levels of growth hormone and IGF-I (somatomedin C) in acromegaly patients who have had inadequate response to or cannot be treated with surgical resection, pituitary irradiation, and bromocriptine mesylate at maximally tolerated doses. The goal is to achieve normalization of growth hormone and IGF-I (somatomedin C) levels. In patients with acromegaly, Octreotide acetate reduces growth hormone to within normal ranges in 50% of patients and reduces IGF-I (somatomedin C) to within normal ranges in 50% to 60% of patients. Since the effects of pituitary irradiation may not become maximal for several years, adjunctive therapy with Octreotide acetate to reduce blood levels of growth hormone and IGF-I (somatomedin C) offers potential benefit before the effects of irradiation are manifested.
Improvement in clinical signs and symptoms or reduction in tumor size or rate of growth were not shown in clinical trials performed with Octreotide acetate; these trials were not optimally designed to detect such effects.
Carcinoid Tumors
Octreotide acetate is indicated for the symptomatic treatment of patients with metastatic carcinoid tumors where it suppresses or inhibits the severe diarrhea and flushing episodes associated with the disease.
Octreotide acetate studies were not designed to show an effect on the size, rate of growth or development of metastases.
Vasoactive Intestinal Peptide Tumors (VIPomas)
Octreotide acetate is indicated for the treatment of the profuse watery diarrhea associated with VIP-secreting tumors. Octreotide acetate studies were not designed to show an effect on the size, rate of growth or development of metastases.
Known hypersensitivity to octreotide or any ingredient in the formulation.
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Known hypersensitivity to octreotide or any ingredient in the formulation.
) [#title] => [#description] => [#children] =>Known hypersensitivity to octreotide or any ingredient in the formulation.
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_contraindications [#title] => Contraindications [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Known hypersensitivity to octreotide or any ingredient in the formulation.
[#printed] => 1 ) [#title] => [#description] => [#children] =>Known hypersensitivity to octreotide or any ingredient in the formulation.
Octreotide acetate alters the balance between the counter-regulatory hormones, insulin, glucagon and growth hormone, which may result in hypoglycemia or hyperglycemia. Octreotide acetate also suppresses secretion of thyroid stimulating hormone, which may result in hypothyroidism. Cardiac conduction abnormalities have also occurred during treatment with Octreotide acetate. However, the incidence of these adverse events during long-term therapy was determined vigorously only in acromegaly patients who, due to their underlying disease and/or the subsequent treatment they receive, are at an increased risk for the development of diabetes mellitus, hypothyroidism, and cardiovascular disease. Although the degree to which these abnormalities are related to Octreotide acetate therapy is not clear, new abnormalities of glycemic control, thyroid function and ECG developed during Octreotide acetate therapy as described below.
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Octreotide acetate alters the balance between the counter-regulatory hormones, insulin, glucagon and growth hormone, which may result in hypoglycemia or hyperglycemia. Octreotide acetate also suppresses secretion of thyroid stimulating hormone, which may result in hypothyroidism. Cardiac conduction abnormalities have also occurred during treatment with Octreotide acetate. However, the incidence of these adverse events during long-term therapy was determined vigorously only in acromegaly patients who, due to their underlying disease and/or the subsequent treatment they receive, are at an increased risk for the development of diabetes mellitus, hypothyroidism, and cardiovascular disease. Although the degree to which these abnormalities are related to Octreotide acetate therapy is not clear, new abnormalities of glycemic control, thyroid function and ECG developed during Octreotide acetate therapy as described below.
) [#title] => [#description] => [#children] =>Octreotide acetate alters the balance between the counter-regulatory hormones, insulin, glucagon and growth hormone, which may result in hypoglycemia or hyperglycemia. Octreotide acetate also suppresses secretion of thyroid stimulating hormone, which may result in hypothyroidism. Cardiac conduction abnormalities have also occurred during treatment with Octreotide acetate. However, the incidence of these adverse events during long-term therapy was determined vigorously only in acromegaly patients who, due to their underlying disease and/or the subsequent treatment they receive, are at an increased risk for the development of diabetes mellitus, hypothyroidism, and cardiovascular disease. Although the degree to which these abnormalities are related to Octreotide acetate therapy is not clear, new abnormalities of glycemic control, thyroid function and ECG developed during Octreotide acetate therapy as described below.
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_precautions [#title] => Precautions [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Octreotide acetate alters the balance between the counter-regulatory hormones, insulin, glucagon and growth hormone, which may result in hypoglycemia or hyperglycemia. Octreotide acetate also suppresses secretion of thyroid stimulating hormone, which may result in hypothyroidism. Cardiac conduction abnormalities have also occurred during treatment with Octreotide acetate. However, the incidence of these adverse events during long-term therapy was determined vigorously only in acromegaly patients who, due to their underlying disease and/or the subsequent treatment they receive, are at an increased risk for the development of diabetes mellitus, hypothyroidism, and cardiovascular disease. Although the degree to which these abnormalities are related to Octreotide acetate therapy is not clear, new abnormalities of glycemic control, thyroid function and ECG developed during Octreotide acetate therapy as described below.
[#printed] => 1 ) [#title] => [#description] => [#children] =>Octreotide acetate alters the balance between the counter-regulatory hormones, insulin, glucagon and growth hormone, which may result in hypoglycemia or hyperglycemia. Octreotide acetate also suppresses secretion of thyroid stimulating hormone, which may result in hypothyroidism. Cardiac conduction abnormalities have also occurred during treatment with Octreotide acetate. However, the incidence of these adverse events during long-term therapy was determined vigorously only in acromegaly patients who, due to their underlying disease and/or the subsequent treatment they receive, are at an increased risk for the development of diabetes mellitus, hypothyroidism, and cardiovascular disease. Although the degree to which these abnormalities are related to Octreotide acetate therapy is not clear, new abnormalities of glycemic control, thyroid function and ECG developed during Octreotide acetate therapy as described below.
Octreotide acetate has been associated with alterations in nutrient absorption, so it may have an effect on absorption of orally administered drugs. Concomitant administration of Octreotide acetate with cyclosporine may decrease blood levels of cyclosporine and result in transplant rejection.
Patients receiving insulin, oral hypoglycemic agents, beta blockers, calcium channel blockers, or agents to control fluid and electrolyte balance, may require dose adjustments of these therapeutic agents.
Concomitant administration of Octreotide and bromocriptine increases the availability of bromocriptine. Limited published data indicate that somatostatin analogs might decrease the metabolic clearance of compounds known to be metabolized by cytochrome P450 enzymes, which may be due to the suppression of growth hormones. Since it cannot be excluded that Octreotide may have this effect, other drugs mainly metabolized by CYP3A4 and which have a low therapeutic index (e.g., quinidine, terfenadine) should therefore be used with caution.
Octreotide acetate has been associated with alterations in nutrient absorption, so it may have an effect on absorption of orally administered drugs. Concomitant administration of Octreotide acetate with cyclosporine may decrease blood levels of cyclosporine and result in transplant rejection.
Patients receiving insulin, oral hypoglycemic agents, beta blockers, calcium channel blockers, or agents to control fluid and electrolyte balance, may require dose adjustments of these therapeutic agents.
Concomitant administration of Octreotide and bromocriptine increases the availability of bromocriptine. Limited published data indicate that somatostatin analogs might decrease the metabolic clearance of compounds known to be metabolized by cytochrome P450 enzymes, which may be due to the suppression of growth hormones. Since it cannot be excluded that Octreotide may have this effect, other drugs mainly metabolized by CYP3A4 and which have a low therapeutic index (e.g., quinidine, terfenadine) should therefore be used with caution.
Octreotide acetate has been associated with alterations in nutrient absorption, so it may have an effect on absorption of orally administered drugs. Concomitant administration of Octreotide acetate with cyclosporine may decrease blood levels of cyclosporine and result in transplant rejection.
Patients receiving insulin, oral hypoglycemic agents, beta blockers, calcium channel blockers, or agents to control fluid and electrolyte balance, may require dose adjustments of these therapeutic agents.
Concomitant administration of Octreotide and bromocriptine increases the availability of bromocriptine. Limited published data indicate that somatostatin analogs might decrease the metabolic clearance of compounds known to be metabolized by cytochrome P450 enzymes, which may be due to the suppression of growth hormones. Since it cannot be excluded that Octreotide may have this effect, other drugs mainly metabolized by CYP3A4 and which have a low therapeutic index (e.g., quinidine, terfenadine) should therefore be used with caution.
Octreotide acetate has been associated with alterations in nutrient absorption, so it may have an effect on absorption of orally administered drugs. Concomitant administration of Octreotide acetate with cyclosporine may decrease blood levels of cyclosporine and result in transplant rejection.
Patients receiving insulin, oral hypoglycemic agents, beta blockers, calcium channel blockers, or agents to control fluid and electrolyte balance, may require dose adjustments of these therapeutic agents.
Concomitant administration of Octreotide and bromocriptine increases the availability of bromocriptine. Limited published data indicate that somatostatin analogs might decrease the metabolic clearance of compounds known to be metabolized by cytochrome P450 enzymes, which may be due to the suppression of growth hormones. Since it cannot be excluded that Octreotide may have this effect, other drugs mainly metabolized by CYP3A4 and which have a low therapeutic index (e.g., quinidine, terfenadine) should therefore be used with caution.
Octreotide acetate has been associated with alterations in nutrient absorption, so it may have an effect on absorption of orally administered drugs. Concomitant administration of Octreotide acetate with cyclosporine may decrease blood levels of cyclosporine and result in transplant rejection.
Patients receiving insulin, oral hypoglycemic agents, beta blockers, calcium channel blockers, or agents to control fluid and electrolyte balance, may require dose adjustments of these therapeutic agents.
Concomitant administration of Octreotide and bromocriptine increases the availability of bromocriptine. Limited published data indicate that somatostatin analogs might decrease the metabolic clearance of compounds known to be metabolized by cytochrome P450 enzymes, which may be due to the suppression of growth hormones. Since it cannot be excluded that Octreotide may have this effect, other drugs mainly metabolized by CYP3A4 and which have a low therapeutic index (e.g., quinidine, terfenadine) should therefore be used with caution.
Gallbladder Abnormalities
Gallbladder abnormalities, especially stones and/or biliary sludge, frequently develop in patients on chronic Octreotide acetate therapy .
Cardiac
In acromegalics, sinus bradycardia (<50 bpm) developed in 25%; conduction abnormalities occurred in 10% and arrhythmias developed in 9% of patients during Octreotide acetate therapy.
Gastrointestinal
Diarrhea, loose stools, nausea and abdominal discomfort were each seen in 34% to 61% of acromegalic patients in U.S. studies although only 2.6% of the patients discontinued therapy due to these symptoms. These symptoms were seen in 5% to 10% of patients with other disorders.
The frequency of these symptoms was not dose-related, but diarrhea and abdominal discomfort generally resolved more quickly in patients treated with 300 mcg/day than in those treated with 750 mcg/day. Vomiting, flatulence, abnormal stools, abdominal distention, and constipation were each seen in less than 10% of patients.
In rare instances, gastrointestinal side effects may resemble acute intestinal obstruction, with progressive abdominal distension, severe epigastric pain, abdominal tenderness and guarding.
Hypo/Hyperglycemia
Hypoglycemia and hyperglycemia occurred in 3% and 16% of acromegalic patients, respectively, but only in about 1.5% of other patients. Symptoms of hypoglycemia were noted in approximately 2% of patients.
Hypothyroidism
In acromegalics, biochemical hypothyroidism alone occurred in 12% while goiter occurred in 6% during Octreotide acetate therapy. In patients without acromegaly, hypothyroidism has only been reported in several isolated patients and goiter has not been reported.
Other Adverse Events
Pain on injection was reported in 7.7%, headache in 6% and dizziness in 5%. Pancreatitis was also observed.
Gallbladder Abnormalities
Gallbladder abnormalities, especially stones and/or biliary sludge, frequently develop in patients on chronic Octreotide acetate therapy .
Cardiac
In acromegalics, sinus bradycardia (<50 bpm) developed in 25%; conduction abnormalities occurred in 10% and arrhythmias developed in 9% of patients during Octreotide acetate therapy.
Gastrointestinal
Diarrhea, loose stools, nausea and abdominal discomfort were each seen in 34% to 61% of acromegalic patients in U.S. studies although only 2.6% of the patients discontinued therapy due to these symptoms. These symptoms were seen in 5% to 10% of patients with other disorders.
The frequency of these symptoms was not dose-related, but diarrhea and abdominal discomfort generally resolved more quickly in patients treated with 300 mcg/day than in those treated with 750 mcg/day. Vomiting, flatulence, abnormal stools, abdominal distention, and constipation were each seen in less than 10% of patients.
In rare instances, gastrointestinal side effects may resemble acute intestinal obstruction, with progressive abdominal distension, severe epigastric pain, abdominal tenderness and guarding.
Hypo/Hyperglycemia
Hypoglycemia and hyperglycemia occurred in 3% and 16% of acromegalic patients, respectively, but only in about 1.5% of other patients. Symptoms of hypoglycemia were noted in approximately 2% of patients.
Hypothyroidism
In acromegalics, biochemical hypothyroidism alone occurred in 12% while goiter occurred in 6% during Octreotide acetate therapy. In patients without acromegaly, hypothyroidism has only been reported in several isolated patients and goiter has not been reported.
Other Adverse Events
Pain on injection was reported in 7.7%, headache in 6% and dizziness in 5%. Pancreatitis was also observed.
Gallbladder Abnormalities
Gallbladder abnormalities, especially stones and/or biliary sludge, frequently develop in patients on chronic Octreotide acetate therapy .
Cardiac
In acromegalics, sinus bradycardia (<50 bpm) developed in 25%; conduction abnormalities occurred in 10% and arrhythmias developed in 9% of patients during Octreotide acetate therapy.
Gastrointestinal
Diarrhea, loose stools, nausea and abdominal discomfort were each seen in 34% to 61% of acromegalic patients in U.S. studies although only 2.6% of the patients discontinued therapy due to these symptoms. These symptoms were seen in 5% to 10% of patients with other disorders.
The frequency of these symptoms was not dose-related, but diarrhea and abdominal discomfort generally resolved more quickly in patients treated with 300 mcg/day than in those treated with 750 mcg/day. Vomiting, flatulence, abnormal stools, abdominal distention, and constipation were each seen in less than 10% of patients.
In rare instances, gastrointestinal side effects may resemble acute intestinal obstruction, with progressive abdominal distension, severe epigastric pain, abdominal tenderness and guarding.
Hypo/Hyperglycemia
Hypoglycemia and hyperglycemia occurred in 3% and 16% of acromegalic patients, respectively, but only in about 1.5% of other patients. Symptoms of hypoglycemia were noted in approximately 2% of patients.
Hypothyroidism
In acromegalics, biochemical hypothyroidism alone occurred in 12% while goiter occurred in 6% during Octreotide acetate therapy. In patients without acromegaly, hypothyroidism has only been reported in several isolated patients and goiter has not been reported.
Other Adverse Events
Pain on injection was reported in 7.7%, headache in 6% and dizziness in 5%. Pancreatitis was also observed.
Gallbladder Abnormalities
Gallbladder abnormalities, especially stones and/or biliary sludge, frequently develop in patients on chronic Octreotide acetate therapy .
Cardiac
In acromegalics, sinus bradycardia (<50 bpm) developed in 25%; conduction abnormalities occurred in 10% and arrhythmias developed in 9% of patients during Octreotide acetate therapy.
Gastrointestinal
Diarrhea, loose stools, nausea and abdominal discomfort were each seen in 34% to 61% of acromegalic patients in U.S. studies although only 2.6% of the patients discontinued therapy due to these symptoms. These symptoms were seen in 5% to 10% of patients with other disorders.
The frequency of these symptoms was not dose-related, but diarrhea and abdominal discomfort generally resolved more quickly in patients treated with 300 mcg/day than in those treated with 750 mcg/day. Vomiting, flatulence, abnormal stools, abdominal distention, and constipation were each seen in less than 10% of patients.
In rare instances, gastrointestinal side effects may resemble acute intestinal obstruction, with progressive abdominal distension, severe epigastric pain, abdominal tenderness and guarding.
Hypo/Hyperglycemia
Hypoglycemia and hyperglycemia occurred in 3% and 16% of acromegalic patients, respectively, but only in about 1.5% of other patients. Symptoms of hypoglycemia were noted in approximately 2% of patients.
Hypothyroidism
In acromegalics, biochemical hypothyroidism alone occurred in 12% while goiter occurred in 6% during Octreotide acetate therapy. In patients without acromegaly, hypothyroidism has only been reported in several isolated patients and goiter has not been reported.
Other Adverse Events
Pain on injection was reported in 7.7%, headache in 6% and dizziness in 5%. Pancreatitis was also observed.
Gallbladder Abnormalities
Gallbladder abnormalities, especially stones and/or biliary sludge, frequently develop in patients on chronic Octreotide acetate therapy .
Cardiac
In acromegalics, sinus bradycardia (<50 bpm) developed in 25%; conduction abnormalities occurred in 10% and arrhythmias developed in 9% of patients during Octreotide acetate therapy.
Gastrointestinal
Diarrhea, loose stools, nausea and abdominal discomfort were each seen in 34% to 61% of acromegalic patients in U.S. studies although only 2.6% of the patients discontinued therapy due to these symptoms. These symptoms were seen in 5% to 10% of patients with other disorders.
The frequency of these symptoms was not dose-related, but diarrhea and abdominal discomfort generally resolved more quickly in patients treated with 300 mcg/day than in those treated with 750 mcg/day. Vomiting, flatulence, abnormal stools, abdominal distention, and constipation were each seen in less than 10% of patients.
In rare instances, gastrointestinal side effects may resemble acute intestinal obstruction, with progressive abdominal distension, severe epigastric pain, abdominal tenderness and guarding.
Hypo/Hyperglycemia
Hypoglycemia and hyperglycemia occurred in 3% and 16% of acromegalic patients, respectively, but only in about 1.5% of other patients. Symptoms of hypoglycemia were noted in approximately 2% of patients.
Hypothyroidism
In acromegalics, biochemical hypothyroidism alone occurred in 12% while goiter occurred in 6% during Octreotide acetate therapy. In patients without acromegaly, hypothyroidism has only been reported in several isolated patients and goiter has not been reported.
Other Adverse Events
Pain on injection was reported in 7.7%, headache in 6% and dizziness in 5%. Pancreatitis was also observed.
Gallbladder Abnormalities
Gallbladder abnormalities, especially stones and/or biliary sludge, frequently develop in patients on chronic Octreotide acetate therapy .
Cardiac
In acromegalics, sinus bradycardia (<50 bpm) developed in 25%; conduction abnormalities occurred in 10% and arrhythmias developed in 9% of patients during Octreotide acetate therapy.
Gastrointestinal
Diarrhea, loose stools, nausea and abdominal discomfort were each seen in 34% to 61% of acromegalic patients in U.S. studies although only 2.6% of the patients discontinued therapy due to these symptoms. These symptoms were seen in 5% to 10% of patients with other disorders.
The frequency of these symptoms was not dose-related, but diarrhea and abdominal discomfort generally resolved more quickly in patients treated with 300 mcg/day than in those treated with 750 mcg/day. Vomiting, flatulence, abnormal stools, abdominal distention, and constipation were each seen in less than 10% of patients.
In rare instances, gastrointestinal side effects may resemble acute intestinal obstruction, with progressive abdominal distension, severe epigastric pain, abdominal tenderness and guarding.
Hypo/Hyperglycemia
Hypoglycemia and hyperglycemia occurred in 3% and 16% of acromegalic patients, respectively, but only in about 1.5% of other patients. Symptoms of hypoglycemia were noted in approximately 2% of patients.
Hypothyroidism
In acromegalics, biochemical hypothyroidism alone occurred in 12% while goiter occurred in 6% during Octreotide acetate therapy. In patients without acromegaly, hypothyroidism has only been reported in several isolated patients and goiter has not been reported.
Other Adverse Events
Pain on injection was reported in 7.7%, headache in 6% and dizziness in 5%. Pancreatitis was also observed.
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
• Injection 50 mcg/1ml: Box of 5Ampoules
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>• Injection 50 mcg/1ml: Box of 5Ampoules
) [#title] => [#description] => [#children] =>• Injection 50 mcg/1ml: Box of 5Ampoules
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_packing [#title] => Packing [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>• Injection 50 mcg/1ml: Box of 5Ampoules
[#printed] => 1 ) [#title] => [#description] => [#children] =>• Injection 50 mcg/1ml: Box of 5Ampoules
OCTOSTATIN®
Injection 50 mcg/1ml
Pituitary Hormones
Somatostatin Analogue
Category B
Octreotide acetate exerts pharmacologic actions similar to the natural hormone, somatostatin. It is an even more potent inhibitor of growth hormone, glucagon, and insulin than somatostatin. Like somatostatin, it also suppresses LH response to GnRH, decreases splanchnic blood flow, and inhibits release of serotonin, gastrin, vasoactive intestinal peptide, secretin, motilin, and pancreatic polypeptide.
After subcutaneous injection, Octreotide is absorbed rapidly and completely from the injection site. Peak concentrations of 5.2 ng/mL (100-mcg dose) were reached 0.4 hours after dosing. Using a specific radioimmunoassay, intravenous and subcutaneous doses were found to be bioequivalent. Peak concentrations and area under the curve values were dose proportional after intravenous single doses up to 200 mcg and subcutaneous single doses up to 500 mcg and after subcutaneous multiple doses up to 500 mcg t.i.d. (1500 mcg/day).
In healthy volunteers the distribution of Octreotide from plasma was rapid (tα1/2=0.2 h), the volume of distribution (Vdss) was estimated to be 13.6 L, and the total body clearance ranged from 7 L/hr to 10 L/hr. In blood, the distribution into the erythrocytes was found to be negligible and about 65% was bound in the plasma in a concentration-independent manner. Binding was mainly to lipoprotein and, to a lesser extent, to albumin.
The elimination of Octreotide from plasma had an apparent half-life of 1.7 to 1.9 hours compared with 1 to 3 minutes with the natural hormone. The duration of action of Octreotide acetate is variable but extends up to 12 hours depending upon the type of tumor. About 32% of the dose is excreted unchanged into the urine. In an elderly population, dose adjustments may be necessary due to a significant increase in the half-life (46%) and a significant decrease in the clearance (26%) of the drug.
In patients with acromegaly, the pharmacokinetics differ somewhat from those in healthy volunteers. A mean peak concentration of 2.8 ng/mL (100-mcg dose) was reached in 0.7 hours after subcutaneous dosing. The volume of distribution (Vdss) was estimated to be 21.6 ± 8.5 L and the total body clearance was increased to 18 L/h. The mean percent of the drug bound was 41.2%. The disposition and elimination half-lives were similar to normals.
In patients with renal impairment the elimination of Octreotide from plasma was prolonged and total body clearance reduced. In mild renal impairment (ClCR40 to 60 mL/min) Octreotide t1/2 was 2.4 hours and total body clearance was 8.8 L/hr, in moderate impairment (ClCR10 to 39 mL/min) t1/2 was 3.0 hours and total body clearance 7.3 L/hr, and in severely renally impaired patients not requiring dialysis (ClCR<10 mL/min) t1/2 was 3.1 hours and total body clearance was 7.6 L/hr. In patients with severe renal failure requiring dialysis, total body clearance was reduced to about half that found in healthy subjects (from approximately 10 L/hr to 4.5 L/hr).
Patients with liver cirrhosis showed prolonged elimination of drug, with Octreotide t1/2 increasing to 3.7 hr and total body clearance decreasing to 5.9 L/hr, whereas patients with fatty liver disease showed t1/2 increased to 3.4 hr and total body clearance of 8.2 L/hr.
Acromegaly
Octreotide acetate is indicated to reduce blood levels of growth hormone and IGF-I (somatomedin C) in acromegaly patients who have had inadequate response to or cannot be treated with surgical resection, pituitary irradiation, and bromocriptine mesylate at maximally tolerated doses. The goal is to achieve normalization of growth hormone and IGF-I (somatomedin C) levels. In patients with acromegaly, Octreotide acetate reduces growth hormone to within normal ranges in 50% of patients and reduces IGF-I (somatomedin C) to within normal ranges in 50% to 60% of patients. Since the effects of pituitary irradiation may not become maximal for several years, adjunctive therapy with Octreotide acetate to reduce blood levels of growth hormone and IGF-I (somatomedin C) offers potential benefit before the effects of irradiation are manifested.
Improvement in clinical signs and symptoms or reduction in tumor size or rate of growth were not shown in clinical trials performed with Octreotide acetate; these trials were not optimally designed to detect such effects.
Carcinoid Tumors
Octreotide acetate is indicated for the symptomatic treatment of patients with metastatic carcinoid tumors where it suppresses or inhibits the severe diarrhea and flushing episodes associated with the disease.
Octreotide acetate studies were not designed to show an effect on the size, rate of growth or development of metastases.
Vasoactive Intestinal Peptide Tumors (VIPomas)
Octreotide acetate is indicated for the treatment of the profuse watery diarrhea associated with VIP-secreting tumors. Octreotide acetate studies were not designed to show an effect on the size, rate of growth or development of metastases.
Known hypersensitivity to octreotide or any ingredient in the formulation.
Octreotide acetate alters the balance between the counter-regulatory hormones, insulin, glucagon and growth hormone, which may result in hypoglycemia or hyperglycemia. Octreotide acetate also suppresses secretion of thyroid stimulating hormone, which may result in hypothyroidism. Cardiac conduction abnormalities have also occurred during treatment with Octreotide acetate. However, the incidence of these adverse events during long-term therapy was determined vigorously only in acromegaly patients who, due to their underlying disease and/or the subsequent treatment they receive, are at an increased risk for the development of diabetes mellitus, hypothyroidism, and cardiovascular disease. Although the degree to which these abnormalities are related to Octreotide acetate therapy is not clear, new abnormalities of glycemic control, thyroid function and ECG developed during Octreotide acetate therapy as described below.
Octreotide acetate has been associated with alterations in nutrient absorption, so it may have an effect on absorption of orally administered drugs. Concomitant administration of Octreotide acetate with cyclosporine may decrease blood levels of cyclosporine and result in transplant rejection.
Patients receiving insulin, oral hypoglycemic agents, beta blockers, calcium channel blockers, or agents to control fluid and electrolyte balance, may require dose adjustments of these therapeutic agents.
Concomitant administration of Octreotide and bromocriptine increases the availability of bromocriptine. Limited published data indicate that somatostatin analogs might decrease the metabolic clearance of compounds known to be metabolized by cytochrome P450 enzymes, which may be due to the suppression of growth hormones. Since it cannot be excluded that Octreotide may have this effect, other drugs mainly metabolized by CYP3A4 and which have a low therapeutic index (e.g., quinidine, terfenadine) should therefore be used with caution.
Gallbladder Abnormalities
Gallbladder abnormalities, especially stones and/or biliary sludge, frequently develop in patients on chronic Octreotide acetate therapy .
Cardiac
In acromegalics, sinus bradycardia (<50 bpm) developed in 25%; conduction abnormalities occurred in 10% and arrhythmias developed in 9% of patients during Octreotide acetate therapy.
Gastrointestinal
Diarrhea, loose stools, nausea and abdominal discomfort were each seen in 34% to 61% of acromegalic patients in U.S. studies although only 2.6% of the patients discontinued therapy due to these symptoms. These symptoms were seen in 5% to 10% of patients with other disorders.
The frequency of these symptoms was not dose-related, but diarrhea and abdominal discomfort generally resolved more quickly in patients treated with 300 mcg/day than in those treated with 750 mcg/day. Vomiting, flatulence, abnormal stools, abdominal distention, and constipation were each seen in less than 10% of patients.
In rare instances, gastrointestinal side effects may resemble acute intestinal obstruction, with progressive abdominal distension, severe epigastric pain, abdominal tenderness and guarding.
Hypo/Hyperglycemia
Hypoglycemia and hyperglycemia occurred in 3% and 16% of acromegalic patients, respectively, but only in about 1.5% of other patients. Symptoms of hypoglycemia were noted in approximately 2% of patients.
Hypothyroidism
In acromegalics, biochemical hypothyroidism alone occurred in 12% while goiter occurred in 6% during Octreotide acetate therapy. In patients without acromegaly, hypothyroidism has only been reported in several isolated patients and goiter has not been reported.
Other Adverse Events
Pain on injection was reported in 7.7%, headache in 6% and dizziness in 5%. Pancreatitis was also observed.
• Store below 30 C°
• Protect from light and freezing
• Injection 50 mcg/1ml: Box of 5Ampoules