Caspian Products
- Ampoules
- Anlagesics, Anti-inflammatory Drugs
- Antimyasthenics ,Muscle Relaxants
- Antiparkinson Drugs, Antidepressants,Antiepileptics, Anxiolytic Sedative, Hypnotics and Antipsychotics
- Hormonal Drugs
- Antihistamines, Bronchodilators
- Cardiovascular Drugs,Electrolytes
- Corticosteroids
- General Anaesthetics, Local Anaesthetics
- Antibacterials
- Gastrointestinal Drugs
- Nutritional Agents and Vitamins
- Antagonists
- Suppository
- Syrups & Oral Solutions
- Ointments, Creams & Gels
- Vial
- Prefilled Syringe
Pamidronate
Pharmacology
The principal pharmacologic action of Pamidronate disodium is inhibition of bone resorption. Although the mechanism of antiresorptive action is not completely understood, several factors are thought to contribute to this action. Pamidronate disodium adsorbs to calcium phosphate (hydroxyapatite) crystals in bone and may directly block dissolution of this mineral component of bone. In vitro studies also suggest that inhibition of osteoclast activity contributes to inhibition of bone resorption. In animal studies, at doses recommended for the treatment of hypercalcemia, Pamidronate disodium inhibits bone resorption apparently without inhibiting bone formation and mineralization. Of relevance to the treatment of hypercalcemia of malignancy is the finding that Pamidronate disodium inhibits the accelerated bone resorption that results from osteoclast hyperactivity induced by various tumors in animal studies.
Pharmacokinetics:
Distribution
The mean ± SD body retention of Pamidronate was calculated to be 54 ± 16% of the dose over 120 hours.
Metabolism
Pamidronate is not metabolized and is exclusively eliminated by renal excretion.
Excretion
After administration of 30, 60, and 90 mg of Pamidronate disodium over 4 hours, and 90 mg of Pamidronate disodium over 24 hours, an overall mean ± SD of 46 ± 16% of the drug was excreted unchanged in the urine within 120 hours. Cumulative urinary excretion was linearly related to dose. The mean ± SD elimination half-life is 28 ± 7 hours. Mean ± SD total and renal clearances of Pamidronate were 107 ± 50 mL/min and 49 ± 28 mL/min, respectively. The rate of elimination from bone has not been determined.
Indications:
Hypercalcemia of Malignancy
Pamidronate disodium, in conjunction with adequate hydration, is indicated for the treatment of moderate or severe hypercalcemia associated with malignancy, with or without bone metastases. Patients who have either epidermoid or non-epidermoid tumors respond to treatment with Pamidronate disodium. Vigorous saline hydration, an integral part of hypercalcemia therapy, should be initiated promptly and an attempt should be made to restore the urine output to about 2 L/day throughout treatment. Mild or asymptomatic hypercalcemia may be treated with conservative measures (i.e., saline hydration, with or without loop diuretics). Patients should be hydrated adequately throughout the treatment, but overhydration, especially in those patients who have cardiac failure, must be avoided. Diuretic therapy should not be employed prior to correction of hypovolemia. The safety and efficacy of Pamidronate disodium in the treatment of hypercalcemia associated with hyperparathyroidism or with other non-tumor-related conditions has not been established.
Paget's Disease
Pamidronate disodium is indicated for the treatment of patients with moderate to severe Paget's disease of bone. The effectiveness of Pamidronate disodium was demonstrated primarily in patients with serum alkaline phosphatase ≥3 times the upper limit of normal. Pamidronate disodium therapy in patients with Paget's disease has been effective in reducing serum alkaline phosphatase and urinary hydroxyproline levels by ≥50% in at least 50% of patients, and by ≥30% in at least 80% of patients. Pamidronate disodium therapy has also been effective in reducing these biochemical markers in patients with Paget's disease who failed to respond, or no longer responded to other treatments.
Osteolytic Bone Metastases of Breast Cancer and Osteolytic Lesions of Multiple Myeloma
Pamidronate disodium is indicated, in conjunction with standard antineoplastic therapy, for the treatment of osteolytic bone metastases of breast cancer and osteolytic lesions of multiple myeloma. The Pamidronate disodium treatment effect appeared to be smaller in the study of breast cancer patients receiving hormonal therapy than in the study of those receiving chemotherapy, however, overall evidence of clinical benefit has been demonstrated.
Contraindications:
Pamidronate disodium is contraindicated in patients with clinically significant hypersensitivity to Pamidronate disodium or other bisphosphonates.
Precautions:
Standard hypercalcemia-related metabolic parameters, such as serum levels of calcium, phosphate, magnesium, and potassium, should be carefully monitored following initiation of therapy with Pamidronate disodium. Cases of asymptomatic hypophosphatemia (12%), hypokalemia (7%), hypomagnesemia (11%), and hypocalcemia (5% to 12%), were reported in Pamidronate disodium-treated patients. Rare cases of symptomatic hypocalcemia (including tetany) have been reported in association with Pamidronate therapy. If hypocalcemia occurs, short-term calcium therapy may be necessary. In Paget's disease of bone, 17% of patients treated with 90 mg of Pamidronate disodium showed serum calcium levels below 8 mg/dL.
Patients with a history of thyroid surgery may have relative hypoparathyroidism that may predispose to hypocalcemia with Pamidronate disodium.
Renal Insufficiency
Pamidronate disodium is excreted intact primarily via the kidney, and the risk of renal adverse reactions may be greater in patients with impaired renal function. Patients who receive Pamidronate disodium should have serum creatinine assessed prior to each treatment. In patients receiving Pamidronate disodium for bone metastases, who show evidence of deterioration in renal function, Pamidronate disodium treatment should be withheld until renal function returns to baseline.
In clinical trials, patients with renal impairment (serum creatinine >3.0 mg/dL) have not been studied. Limited pharmacokinetic data exist in patients with creatinine clearance <30 mL/min For the treatment of bone metastases, the use of Pamidronate disodium in patients with severe renal impairment is not recommended. In other indications, clinical judgement should determine whether the potential benefit outweighs the potential risk in such patients.
Osteonecrosis of the Jaw
Osteonecrosis of the jaw (ONJ) has been reported predominantly in cancer patients treated with intravenous biphosphonates, including Pamidronate disodium. Many of these patients were also receiving chemotherapy and corticosteroids which may be risk factors for ONJ. Postmarketing experience and the literature suggests a greater frequency of reports of ONJ based on tumor type (advanced breast cancer, multiple myeloma), and dental status (dental extraction, periodontal disease, local trauma including poorly fitting dentures). Many reports of ONJ involved patients with signs of local infection including osteomyelitis.
Cancer patients should maintain good oral hygiene and should have a dental examination with preventive dentistry prior to treatment with bisphophonates.
While on treatment, these patients should avoid invasive dental procedures if possible. For patients who develop ONJ while on bisphosphonate therapy, dental surgery may exacerbate the condition. For patients requiring dental procedures, there are no data available to suggest whether discontinuation of bisphosphonate treatment reduces the risk of ONJ. Clinical judgement of the treating physician should guide the management plan of each patient based on individual benefit/risk assessment.
Drug Interactions:
Pamidronate can harm your kidneys. This effect is increased when you also use other medicines harmful to the kidneys. You may need dose adjustments or special tests if you have recently used:
• lithium
• methotrexate
• pain or arthritis medicines such as aspirin, acetaminophen, diclofenac, etodolac , ibuprofen, indomethacin, naproxen, and others
• medicines used to treat ulcerative colitis, such as mesalamine (Pentasa) or sulfasalazine
• medicines used to prevent organ transplant rejection, such as cyclosporine (Neoral, Sandimmune), sirolimus (Rapamune) or tacrolimus (Prograf)
• IV antibiotics such as amphotericin B (Fungizone), amikacin, bacitracin, capreomycin, gentamicin, kanamycin, streptomycin, or vancomycin
• antiviral medicines such as adefovir (Hepsera), cidofovir, or foscarnet (Foscavir); or
• cancer medicine such as aldesleukin, carmustine (BiCNU), cisplatin, ifosfamide, oxaliplatin (Eloxatin), streptozocin, or tretinoin
Side Effects:
• high fever;
• severe joint, bone, or muscle pain;
• new or unusual pain in your thigh or hip;
• urinating less than usual or not at all;
• swelling, rapid weight gain;
• pain or burning when you urinate;
• seizure (convulsions);
• eye pain, vision changes;
• pale skin, feeling light-headed or short of breath, rapid heart rate, trouble concentrating; or
• confusion, uneven heart rate, extreme thirst, increased urination, leg discomfort, muscle weakness or limp feeling, or jerking muscle movements.
• low fever;
• stomach pain, loss of appetite, nausea, vomiting;
• constipation; or
• pain, redness, swelling or a hard painful lump under your skin around the IV needle.
Storage:
• Store below 30 C°
• Protect from light and freezing
Packing:
• Injection 90mg/10ml: Box of 1Ampoule
PAMIDATE®
Injection 90mg/10ml
Bisphosphonates
Bone modulating drugs
Category D
The principal pharmacologic action of Pamidronate disodium is inhibition of bone resorption. Although the mechanism of antiresorptive action is not completely understood, several factors are thought to contribute to this action. Pamidronate disodium adsorbs to calcium phosphate (hydroxyapatite) crystals in bone and may directly block dissolution of this mineral component of bone. In vitro studies also suggest that inhibition of osteoclast activity contributes to inhibition of bone resorption. In animal studies, at doses recommended for the treatment of hypercalcemia, Pamidronate disodium inhibits bone resorption apparently without inhibiting bone formation and mineralization. Of relevance to the treatment of hypercalcemia of malignancy is the finding that Pamidronate disodium inhibits the accelerated bone resorption that results from osteoclast hyperactivity induced by various tumors in animal studies.
Distribution
The mean ± SD body retention of Pamidronate was calculated to be 54 ± 16% of the dose over 120 hours.
Metabolism
Pamidronate is not metabolized and is exclusively eliminated by renal excretion.
Excretion
After administration of 30, 60, and 90 mg of Pamidronate disodium over 4 hours, and 90 mg of Pamidronate disodium over 24 hours, an overall mean ± SD of 46 ± 16% of the drug was excreted unchanged in the urine within 120 hours. Cumulative urinary excretion was linearly related to dose. The mean ± SD elimination half-life is 28 ± 7 hours. Mean ± SD total and renal clearances of Pamidronate were 107 ± 50 mL/min and 49 ± 28 mL/min, respectively. The rate of elimination from bone has not been determined.
Hypercalcemia of Malignancy
Pamidronate disodium, in conjunction with adequate hydration, is indicated for the treatment of moderate or severe hypercalcemia associated with malignancy, with or without bone metastases. Patients who have either epidermoid or non-epidermoid tumors respond to treatment with Pamidronate disodium. Vigorous saline hydration, an integral part of hypercalcemia therapy, should be initiated promptly and an attempt should be made to restore the urine output to about 2 L/day throughout treatment. Mild or asymptomatic hypercalcemia may be treated with conservative measures (i.e., saline hydration, with or without loop diuretics). Patients should be hydrated adequately throughout the treatment, but overhydration, especially in those patients who have cardiac failure, must be avoided. Diuretic therapy should not be employed prior to correction of hypovolemia. The safety and efficacy of Pamidronate disodium in the treatment of hypercalcemia associated with hyperparathyroidism or with other non-tumor-related conditions has not been established.
Paget's Disease
Pamidronate disodium is indicated for the treatment of patients with moderate to severe Paget's disease of bone. The effectiveness of Pamidronate disodium was demonstrated primarily in patients with serum alkaline phosphatase ≥3 times the upper limit of normal. Pamidronate disodium therapy in patients with Paget's disease has been effective in reducing serum alkaline phosphatase and urinary hydroxyproline levels by ≥50% in at least 50% of patients, and by ≥30% in at least 80% of patients. Pamidronate disodium therapy has also been effective in reducing these biochemical markers in patients with Paget's disease who failed to respond, or no longer responded to other treatments.
Osteolytic Bone Metastases of Breast Cancer and Osteolytic Lesions of Multiple Myeloma
Pamidronate disodium is indicated, in conjunction with standard antineoplastic therapy, for the treatment of osteolytic bone metastases of breast cancer and osteolytic lesions of multiple myeloma. The Pamidronate disodium treatment effect appeared to be smaller in the study of breast cancer patients receiving hormonal therapy than in the study of those receiving chemotherapy, however, overall evidence of clinical benefit has been demonstrated.
Pamidronate disodium is contraindicated in patients with clinically significant hypersensitivity to Pamidronate disodium or other bisphosphonates.
Standard hypercalcemia-related metabolic parameters, such as serum levels of calcium, phosphate, magnesium, and potassium, should be carefully monitored following initiation of therapy with Pamidronate disodium. Cases of asymptomatic hypophosphatemia (12%), hypokalemia (7%), hypomagnesemia (11%), and hypocalcemia (5% to 12%), were reported in Pamidronate disodium-treated patients. Rare cases of symptomatic hypocalcemia (including tetany) have been reported in association with Pamidronate therapy. If hypocalcemia occurs, short-term calcium therapy may be necessary. In Paget's disease of bone, 17% of patients treated with 90 mg of Pamidronate disodium showed serum calcium levels below 8 mg/dL.
Patients with a history of thyroid surgery may have relative hypoparathyroidism that may predispose to hypocalcemia with Pamidronate disodium.
Renal Insufficiency
Pamidronate disodium is excreted intact primarily via the kidney, and the risk of renal adverse reactions may be greater in patients with impaired renal function. Patients who receive Pamidronate disodium should have serum creatinine assessed prior to each treatment. In patients receiving Pamidronate disodium for bone metastases, who show evidence of deterioration in renal function, Pamidronate disodium treatment should be withheld until renal function returns to baseline.
In clinical trials, patients with renal impairment (serum creatinine >3.0 mg/dL) have not been studied. Limited pharmacokinetic data exist in patients with creatinine clearance <30 mL/min For the treatment of bone metastases, the use of Pamidronate disodium in patients with severe renal impairment is not recommended. In other indications, clinical judgement should determine whether the potential benefit outweighs the potential risk in such patients.
Osteonecrosis of the Jaw
Osteonecrosis of the jaw (ONJ) has been reported predominantly in cancer patients treated with intravenous biphosphonates, including Pamidronate disodium. Many of these patients were also receiving chemotherapy and corticosteroids which may be risk factors for ONJ. Postmarketing experience and the literature suggests a greater frequency of reports of ONJ based on tumor type (advanced breast cancer, multiple myeloma), and dental status (dental extraction, periodontal disease, local trauma including poorly fitting dentures). Many reports of ONJ involved patients with signs of local infection including osteomyelitis.
Cancer patients should maintain good oral hygiene and should have a dental examination with preventive dentistry prior to treatment with bisphophonates.
While on treatment, these patients should avoid invasive dental procedures if possible. For patients who develop ONJ while on bisphosphonate therapy, dental surgery may exacerbate the condition. For patients requiring dental procedures, there are no data available to suggest whether discontinuation of bisphosphonate treatment reduces the risk of ONJ. Clinical judgement of the treating physician should guide the management plan of each patient based on individual benefit/risk assessment.
Pamidronate can harm your kidneys. This effect is increased when you also use other medicines harmful to the kidneys. You may need dose adjustments or special tests if you have recently used:
• lithium
• methotrexate
• pain or arthritis medicines such as aspirin, acetaminophen, diclofenac, etodolac , ibuprofen, indomethacin, naproxen, and others
• medicines used to treat ulcerative colitis, such as mesalamine (Pentasa) or sulfasalazine
• medicines used to prevent organ transplant rejection, such as cyclosporine (Neoral, Sandimmune), sirolimus (Rapamune) or tacrolimus (Prograf)
• IV antibiotics such as amphotericin B (Fungizone), amikacin, bacitracin, capreomycin, gentamicin, kanamycin, streptomycin, or vancomycin
• antiviral medicines such as adefovir (Hepsera), cidofovir, or foscarnet (Foscavir); or
• cancer medicine such as aldesleukin, carmustine (BiCNU), cisplatin, ifosfamide, oxaliplatin (Eloxatin), streptozocin, or tretinoin
• high fever;
• severe joint, bone, or muscle pain;
• new or unusual pain in your thigh or hip;
• urinating less than usual or not at all;
• swelling, rapid weight gain;
• pain or burning when you urinate;
• seizure (convulsions);
• eye pain, vision changes;
• pale skin, feeling light-headed or short of breath, rapid heart rate, trouble concentrating; or
• confusion, uneven heart rate, extreme thirst, increased urination, leg discomfort, muscle weakness or limp feeling, or jerking muscle movements.
• low fever;
• stomach pain, loss of appetite, nausea, vomiting;
• constipation; or
• pain, redness, swelling or a hard painful lump under your skin around the IV needle.
• Store below 30 C°
• Protect from light and freezing
• Injection 90mg/10ml: Box of 1Ampoule
 )
)
[field_administration_and_dosage] => Array
(
[0] => Array
(
[value] =>
[format] =>
[safe] =>
[view] =>
)
)
[field_brand_name] => Array
(
[0] => Array
(
[value] => PAMIDATE®
[format] => 1
[safe] =>
)
)
[field_administration_and_dosage] => Array
(
[0] => Array
(
[value] =>
[format] =>
[safe] =>
[view] =>
)
)
[field_brand_name] => Array
(
[0] => Array
(
[value] => PAMIDATE®
[format] => 1
[safe] => PAMIDATE®
[view] =>PAMIDATE®
) ) [field_contraindications] => Array ( [0] => Array ( [value] => Pamidronate disodium is contraindicated in patients with clinically significant hypersensitivity to Pamidronate disodium or other bisphosphonates. [format] => 1 [safe] =>Pamidronate disodium is contraindicated in patients with clinically significant hypersensitivity to Pamidronate disodium or other bisphosphonates.
[view] =>Pamidronate disodium is contraindicated in patients with clinically significant hypersensitivity to Pamidronate disodium or other bisphosphonates.
) ) [field_dosage_form] => Array ( [0] => Array ( [value] => Injection 90mg/10ml [format] => 1 [safe] =>Injection 90mg/10ml
[view] =>Injection 90mg/10ml
) ) [field_drug_interactions] => Array ( [0] => Array ( [value] => Pamidronate can harm your kidneys. This effect is increased when you also use other medicines harmful to the kidneys. You may need dose adjustments or special tests if you have recently used: • lithium • methotrexate • pain or arthritis medicines such as aspirin, acetaminophen, diclofenac, etodolac , ibuprofen, indomethacin, naproxen, and others • medicines used to treat ulcerative colitis, such as mesalamine (Pentasa) or sulfasalazine • medicines used to prevent organ transplant rejection, such as cyclosporine (Neoral, Sandimmune), sirolimus (Rapamune) or tacrolimus (Prograf) • IV antibiotics such as amphotericin B (Fungizone), amikacin, bacitracin, capreomycin, gentamicin, kanamycin, streptomycin, or vancomycin • antiviral medicines such as adefovir (Hepsera), cidofovir, or foscarnet (Foscavir); or • cancer medicine such as aldesleukin, carmustine (BiCNU), cisplatin, ifosfamide, oxaliplatin (Eloxatin), streptozocin, or tretinoin [format] => 1 [safe] =>Pamidronate can harm your kidneys. This effect is increased when you also use other medicines harmful to the kidneys. You may need dose adjustments or special tests if you have recently used:
• lithium
• methotrexate
• pain or arthritis medicines such as aspirin, acetaminophen, diclofenac, etodolac , ibuprofen, indomethacin, naproxen, and others
• medicines used to treat ulcerative colitis, such as mesalamine (Pentasa) or sulfasalazine
• medicines used to prevent organ transplant rejection, such as cyclosporine (Neoral, Sandimmune), sirolimus (Rapamune) or tacrolimus (Prograf)
• IV antibiotics such as amphotericin B (Fungizone), amikacin, bacitracin, capreomycin, gentamicin, kanamycin, streptomycin, or vancomycin
• antiviral medicines such as adefovir (Hepsera), cidofovir, or foscarnet (Foscavir); or
• cancer medicine such as aldesleukin, carmustine (BiCNU), cisplatin, ifosfamide, oxaliplatin (Eloxatin), streptozocin, or tretinoin
Pamidronate can harm your kidneys. This effect is increased when you also use other medicines harmful to the kidneys. You may need dose adjustments or special tests if you have recently used:
• lithium
• methotrexate
• pain or arthritis medicines such as aspirin, acetaminophen, diclofenac, etodolac , ibuprofen, indomethacin, naproxen, and others
• medicines used to treat ulcerative colitis, such as mesalamine (Pentasa) or sulfasalazine
• medicines used to prevent organ transplant rejection, such as cyclosporine (Neoral, Sandimmune), sirolimus (Rapamune) or tacrolimus (Prograf)
• IV antibiotics such as amphotericin B (Fungizone), amikacin, bacitracin, capreomycin, gentamicin, kanamycin, streptomycin, or vancomycin
• antiviral medicines such as adefovir (Hepsera), cidofovir, or foscarnet (Foscavir); or
• cancer medicine such as aldesleukin, carmustine (BiCNU), cisplatin, ifosfamide, oxaliplatin (Eloxatin), streptozocin, or tretinoin
Hypercalcemia of Malignancy
Pamidronate disodium, in conjunction with adequate hydration, is indicated for the treatment of moderate or severe hypercalcemia associated with malignancy, with or without bone metastases. Patients who have either epidermoid or non-epidermoid tumors respond to treatment with Pamidronate disodium. Vigorous saline hydration, an integral part of hypercalcemia therapy, should be initiated promptly and an attempt should be made to restore the urine output to about 2 L/day throughout treatment. Mild or asymptomatic hypercalcemia may be treated with conservative measures (i.e., saline hydration, with or without loop diuretics). Patients should be hydrated adequately throughout the treatment, but overhydration, especially in those patients who have cardiac failure, must be avoided. Diuretic therapy should not be employed prior to correction of hypovolemia. The safety and efficacy of Pamidronate disodium in the treatment of hypercalcemia associated with hyperparathyroidism or with other non-tumor-related conditions has not been established.
Paget's Disease
Pamidronate disodium is indicated for the treatment of patients with moderate to severe Paget's disease of bone. The effectiveness of Pamidronate disodium was demonstrated primarily in patients with serum alkaline phosphatase ≥3 times the upper limit of normal. Pamidronate disodium therapy in patients with Paget's disease has been effective in reducing serum alkaline phosphatase and urinary hydroxyproline levels by ≥50% in at least 50% of patients, and by ≥30% in at least 80% of patients. Pamidronate disodium therapy has also been effective in reducing these biochemical markers in patients with Paget's disease who failed to respond, or no longer responded to other treatments.
Osteolytic Bone Metastases of Breast Cancer and Osteolytic Lesions of Multiple Myeloma
Pamidronate disodium is indicated, in conjunction with standard antineoplastic therapy, for the treatment of osteolytic bone metastases of breast cancer and osteolytic lesions of multiple myeloma. The Pamidronate disodium treatment effect appeared to be smaller in the study of breast cancer patients receiving hormonal therapy than in the study of those receiving chemotherapy, however, overall evidence of clinical benefit has been demonstrated.
Hypercalcemia of Malignancy
Pamidronate disodium, in conjunction with adequate hydration, is indicated for the treatment of moderate or severe hypercalcemia associated with malignancy, with or without bone metastases. Patients who have either epidermoid or non-epidermoid tumors respond to treatment with Pamidronate disodium. Vigorous saline hydration, an integral part of hypercalcemia therapy, should be initiated promptly and an attempt should be made to restore the urine output to about 2 L/day throughout treatment. Mild or asymptomatic hypercalcemia may be treated with conservative measures (i.e., saline hydration, with or without loop diuretics). Patients should be hydrated adequately throughout the treatment, but overhydration, especially in those patients who have cardiac failure, must be avoided. Diuretic therapy should not be employed prior to correction of hypovolemia. The safety and efficacy of Pamidronate disodium in the treatment of hypercalcemia associated with hyperparathyroidism or with other non-tumor-related conditions has not been established.
Paget's Disease
Pamidronate disodium is indicated for the treatment of patients with moderate to severe Paget's disease of bone. The effectiveness of Pamidronate disodium was demonstrated primarily in patients with serum alkaline phosphatase ≥3 times the upper limit of normal. Pamidronate disodium therapy in patients with Paget's disease has been effective in reducing serum alkaline phosphatase and urinary hydroxyproline levels by ≥50% in at least 50% of patients, and by ≥30% in at least 80% of patients. Pamidronate disodium therapy has also been effective in reducing these biochemical markers in patients with Paget's disease who failed to respond, or no longer responded to other treatments.
Osteolytic Bone Metastases of Breast Cancer and Osteolytic Lesions of Multiple Myeloma
Pamidronate disodium is indicated, in conjunction with standard antineoplastic therapy, for the treatment of osteolytic bone metastases of breast cancer and osteolytic lesions of multiple myeloma. The Pamidronate disodium treatment effect appeared to be smaller in the study of breast cancer patients receiving hormonal therapy than in the study of those receiving chemotherapy, however, overall evidence of clinical benefit has been demonstrated.
Hypercalcemia of Malignancy
Pamidronate disodium, in conjunction with adequate hydration, is indicated for the treatment of moderate or severe hypercalcemia associated with malignancy, with or without bone metastases. Patients who have either epidermoid or non-epidermoid tumors respond to treatment with Pamidronate disodium. Vigorous saline hydration, an integral part of hypercalcemia therapy, should be initiated promptly and an attempt should be made to restore the urine output to about 2 L/day throughout treatment. Mild or asymptomatic hypercalcemia may be treated with conservative measures (i.e., saline hydration, with or without loop diuretics). Patients should be hydrated adequately throughout the treatment, but overhydration, especially in those patients who have cardiac failure, must be avoided. Diuretic therapy should not be employed prior to correction of hypovolemia. The safety and efficacy of Pamidronate disodium in the treatment of hypercalcemia associated with hyperparathyroidism or with other non-tumor-related conditions has not been established.
Paget's Disease
Pamidronate disodium is indicated for the treatment of patients with moderate to severe Paget's disease of bone. The effectiveness of Pamidronate disodium was demonstrated primarily in patients with serum alkaline phosphatase ≥3 times the upper limit of normal. Pamidronate disodium therapy in patients with Paget's disease has been effective in reducing serum alkaline phosphatase and urinary hydroxyproline levels by ≥50% in at least 50% of patients, and by ≥30% in at least 80% of patients. Pamidronate disodium therapy has also been effective in reducing these biochemical markers in patients with Paget's disease who failed to respond, or no longer responded to other treatments.
Osteolytic Bone Metastases of Breast Cancer and Osteolytic Lesions of Multiple Myeloma
Pamidronate disodium is indicated, in conjunction with standard antineoplastic therapy, for the treatment of osteolytic bone metastases of breast cancer and osteolytic lesions of multiple myeloma. The Pamidronate disodium treatment effect appeared to be smaller in the study of breast cancer patients receiving hormonal therapy than in the study of those receiving chemotherapy, however, overall evidence of clinical benefit has been demonstrated.
• Injection 90mg/10ml: Box of 1Ampoule
[view] =>• Injection 90mg/10ml: Box of 1Ampoule
) ) [field_pdf] => Array ( [0] => Array ( [fid] => 238 [uid] => 1 [filename] => pamidronate.pdf [filepath] => sites/default/files/pdf/pamidronate.pdf [filemime] => application/pdf [filesize] => 115442 [status] => 1 [timestamp] => 1329504227 [list] => 1 [data] => [i18nsync] => 1 [nid] => 264 [view] => ) ) [field_pharmacokinetics] => Array ( [0] => Array ( [value] =>Distribution
The mean ± SD body retention of Pamidronate was calculated to be 54 ± 16% of the dose over 120 hours.
Metabolism
Pamidronate is not metabolized and is exclusively eliminated by renal excretion.
Excretion
After administration of 30, 60, and 90 mg of Pamidronate disodium over 4 hours, and 90 mg of Pamidronate disodium over 24 hours, an overall mean ± SD of 46 ± 16% of the drug was excreted unchanged in the urine within 120 hours. Cumulative urinary excretion was linearly related to dose. The mean ± SD elimination half-life is 28 ± 7 hours. Mean ± SD total and renal clearances of Pamidronate were 107 ± 50 mL/min and 49 ± 28 mL/min, respectively. The rate of elimination from bone has not been determined.
Distribution
The mean ± SD body retention of Pamidronate was calculated to be 54 ± 16% of the dose over 120 hours.
Metabolism
Pamidronate is not metabolized and is exclusively eliminated by renal excretion.
Excretion
After administration of 30, 60, and 90 mg of Pamidronate disodium over 4 hours, and 90 mg of Pamidronate disodium over 24 hours, an overall mean ± SD of 46 ± 16% of the drug was excreted unchanged in the urine within 120 hours. Cumulative urinary excretion was linearly related to dose. The mean ± SD elimination half-life is 28 ± 7 hours. Mean ± SD total and renal clearances of Pamidronate were 107 ± 50 mL/min and 49 ± 28 mL/min, respectively. The rate of elimination from bone has not been determined.
Distribution
The mean ± SD body retention of Pamidronate was calculated to be 54 ± 16% of the dose over 120 hours.
Metabolism
Pamidronate is not metabolized and is exclusively eliminated by renal excretion.
Excretion
After administration of 30, 60, and 90 mg of Pamidronate disodium over 4 hours, and 90 mg of Pamidronate disodium over 24 hours, an overall mean ± SD of 46 ± 16% of the drug was excreted unchanged in the urine within 120 hours. Cumulative urinary excretion was linearly related to dose. The mean ± SD elimination half-life is 28 ± 7 hours. Mean ± SD total and renal clearances of Pamidronate were 107 ± 50 mL/min and 49 ± 28 mL/min, respectively. The rate of elimination from bone has not been determined.
Bisphosphonates
[view] =>Bisphosphonates
) ) [field_precautions] => Array ( [0] => Array ( [value] =>Standard hypercalcemia-related metabolic parameters, such as serum levels of calcium, phosphate, magnesium, and potassium, should be carefully monitored following initiation of therapy with Pamidronate disodium. Cases of asymptomatic hypophosphatemia (12%), hypokalemia (7%), hypomagnesemia (11%), and hypocalcemia (5% to 12%), were reported in Pamidronate disodium-treated patients. Rare cases of symptomatic hypocalcemia (including tetany) have been reported in association with Pamidronate therapy. If hypocalcemia occurs, short-term calcium therapy may be necessary. In Paget's disease of bone, 17% of patients treated with 90 mg of Pamidronate disodium showed serum calcium levels below 8 mg/dL.
Patients with a history of thyroid surgery may have relative hypoparathyroidism that may predispose to hypocalcemia with Pamidronate disodium.
Renal Insufficiency
Pamidronate disodium is excreted intact primarily via the kidney, and the risk of renal adverse reactions may be greater in patients with impaired renal function. Patients who receive Pamidronate disodium should have serum creatinine assessed prior to each treatment. In patients receiving Pamidronate disodium for bone metastases, who show evidence of deterioration in renal function, Pamidronate disodium treatment should be withheld until renal function returns to baseline.
In clinical trials, patients with renal impairment (serum creatinine >3.0 mg/dL) have not been studied. Limited pharmacokinetic data exist in patients with creatinine clearance <30 mL/min For the treatment of bone metastases, the use of Pamidronate disodium in patients with severe renal impairment is not recommended. In other indications, clinical judgement should determine whether the potential benefit outweighs the potential risk in such patients.
Osteonecrosis of the Jaw
Osteonecrosis of the jaw (ONJ) has been reported predominantly in cancer patients treated with intravenous biphosphonates, including Pamidronate disodium. Many of these patients were also receiving chemotherapy and corticosteroids which may be risk factors for ONJ. Postmarketing experience and the literature suggests a greater frequency of reports of ONJ based on tumor type (advanced breast cancer, multiple myeloma), and dental status (dental extraction, periodontal disease, local trauma including poorly fitting dentures). Many reports of ONJ involved patients with signs of local infection including osteomyelitis.
Cancer patients should maintain good oral hygiene and should have a dental examination with preventive dentistry prior to treatment with bisphophonates.
While on treatment, these patients should avoid invasive dental procedures if possible. For patients who develop ONJ while on bisphosphonate therapy, dental surgery may exacerbate the condition. For patients requiring dental procedures, there are no data available to suggest whether discontinuation of bisphosphonate treatment reduces the risk of ONJ. Clinical judgement of the treating physician should guide the management plan of each patient based on individual benefit/risk assessment.
Standard hypercalcemia-related metabolic parameters, such as serum levels of calcium, phosphate, magnesium, and potassium, should be carefully monitored following initiation of therapy with Pamidronate disodium. Cases of asymptomatic hypophosphatemia (12%), hypokalemia (7%), hypomagnesemia (11%), and hypocalcemia (5% to 12%), were reported in Pamidronate disodium-treated patients. Rare cases of symptomatic hypocalcemia (including tetany) have been reported in association with Pamidronate therapy. If hypocalcemia occurs, short-term calcium therapy may be necessary. In Paget's disease of bone, 17% of patients treated with 90 mg of Pamidronate disodium showed serum calcium levels below 8 mg/dL.
Patients with a history of thyroid surgery may have relative hypoparathyroidism that may predispose to hypocalcemia with Pamidronate disodium.
Renal Insufficiency
Pamidronate disodium is excreted intact primarily via the kidney, and the risk of renal adverse reactions may be greater in patients with impaired renal function. Patients who receive Pamidronate disodium should have serum creatinine assessed prior to each treatment. In patients receiving Pamidronate disodium for bone metastases, who show evidence of deterioration in renal function, Pamidronate disodium treatment should be withheld until renal function returns to baseline.
In clinical trials, patients with renal impairment (serum creatinine >3.0 mg/dL) have not been studied. Limited pharmacokinetic data exist in patients with creatinine clearance <30 mL/min For the treatment of bone metastases, the use of Pamidronate disodium in patients with severe renal impairment is not recommended. In other indications, clinical judgement should determine whether the potential benefit outweighs the potential risk in such patients.
Osteonecrosis of the Jaw
Osteonecrosis of the jaw (ONJ) has been reported predominantly in cancer patients treated with intravenous biphosphonates, including Pamidronate disodium. Many of these patients were also receiving chemotherapy and corticosteroids which may be risk factors for ONJ. Postmarketing experience and the literature suggests a greater frequency of reports of ONJ based on tumor type (advanced breast cancer, multiple myeloma), and dental status (dental extraction, periodontal disease, local trauma including poorly fitting dentures). Many reports of ONJ involved patients with signs of local infection including osteomyelitis.
Cancer patients should maintain good oral hygiene and should have a dental examination with preventive dentistry prior to treatment with bisphophonates.
While on treatment, these patients should avoid invasive dental procedures if possible. For patients who develop ONJ while on bisphosphonate therapy, dental surgery may exacerbate the condition. For patients requiring dental procedures, there are no data available to suggest whether discontinuation of bisphosphonate treatment reduces the risk of ONJ. Clinical judgement of the treating physician should guide the management plan of each patient based on individual benefit/risk assessment.
Standard hypercalcemia-related metabolic parameters, such as serum levels of calcium, phosphate, magnesium, and potassium, should be carefully monitored following initiation of therapy with Pamidronate disodium. Cases of asymptomatic hypophosphatemia (12%), hypokalemia (7%), hypomagnesemia (11%), and hypocalcemia (5% to 12%), were reported in Pamidronate disodium-treated patients. Rare cases of symptomatic hypocalcemia (including tetany) have been reported in association with Pamidronate therapy. If hypocalcemia occurs, short-term calcium therapy may be necessary. In Paget's disease of bone, 17% of patients treated with 90 mg of Pamidronate disodium showed serum calcium levels below 8 mg/dL.
Patients with a history of thyroid surgery may have relative hypoparathyroidism that may predispose to hypocalcemia with Pamidronate disodium.
Renal Insufficiency
Pamidronate disodium is excreted intact primarily via the kidney, and the risk of renal adverse reactions may be greater in patients with impaired renal function. Patients who receive Pamidronate disodium should have serum creatinine assessed prior to each treatment. In patients receiving Pamidronate disodium for bone metastases, who show evidence of deterioration in renal function, Pamidronate disodium treatment should be withheld until renal function returns to baseline.
In clinical trials, patients with renal impairment (serum creatinine >3.0 mg/dL) have not been studied. Limited pharmacokinetic data exist in patients with creatinine clearance <30 mL/min For the treatment of bone metastases, the use of Pamidronate disodium in patients with severe renal impairment is not recommended. In other indications, clinical judgement should determine whether the potential benefit outweighs the potential risk in such patients.
Osteonecrosis of the Jaw
Osteonecrosis of the jaw (ONJ) has been reported predominantly in cancer patients treated with intravenous biphosphonates, including Pamidronate disodium. Many of these patients were also receiving chemotherapy and corticosteroids which may be risk factors for ONJ. Postmarketing experience and the literature suggests a greater frequency of reports of ONJ based on tumor type (advanced breast cancer, multiple myeloma), and dental status (dental extraction, periodontal disease, local trauma including poorly fitting dentures). Many reports of ONJ involved patients with signs of local infection including osteomyelitis.
Cancer patients should maintain good oral hygiene and should have a dental examination with preventive dentistry prior to treatment with bisphophonates.
While on treatment, these patients should avoid invasive dental procedures if possible. For patients who develop ONJ while on bisphosphonate therapy, dental surgery may exacerbate the condition. For patients requiring dental procedures, there are no data available to suggest whether discontinuation of bisphosphonate treatment reduces the risk of ONJ. Clinical judgement of the treating physician should guide the management plan of each patient based on individual benefit/risk assessment.
Category D
[view] =>Category D
) ) [field_references] => Array ( [0] => Array ( [value] => [format] => [safe] => [view] => ) ) [field_side_effects] => Array ( [0] => Array ( [value] => • high fever; • severe joint, bone, or muscle pain; • new or unusual pain in your thigh or hip; • urinating less than usual or not at all; • swelling, rapid weight gain; • pain or burning when you urinate; • seizure (convulsions); • eye pain, vision changes; • pale skin, feeling light-headed or short of breath, rapid heart rate, trouble concentrating; or • confusion, uneven heart rate, extreme thirst, increased urination, leg discomfort, muscle weakness or limp feeling, or jerking muscle movements. • low fever; • stomach pain, loss of appetite, nausea, vomiting; • constipation; or • pain, redness, swelling or a hard painful lump under your skin around the IV needle. [format] => 1 [safe] =>• high fever;
• severe joint, bone, or muscle pain;
• new or unusual pain in your thigh or hip;
• urinating less than usual or not at all;
• swelling, rapid weight gain;
• pain or burning when you urinate;
• seizure (convulsions);
• eye pain, vision changes;
• pale skin, feeling light-headed or short of breath, rapid heart rate, trouble concentrating; or
• confusion, uneven heart rate, extreme thirst, increased urination, leg discomfort, muscle weakness or limp feeling, or jerking muscle movements.
• low fever;
• stomach pain, loss of appetite, nausea, vomiting;
• constipation; or
• pain, redness, swelling or a hard painful lump under your skin around the IV needle.
• high fever;
• severe joint, bone, or muscle pain;
• new or unusual pain in your thigh or hip;
• urinating less than usual or not at all;
• swelling, rapid weight gain;
• pain or burning when you urinate;
• seizure (convulsions);
• eye pain, vision changes;
• pale skin, feeling light-headed or short of breath, rapid heart rate, trouble concentrating; or
• confusion, uneven heart rate, extreme thirst, increased urination, leg discomfort, muscle weakness or limp feeling, or jerking muscle movements.
• low fever;
• stomach pain, loss of appetite, nausea, vomiting;
• constipation; or
• pain, redness, swelling or a hard painful lump under your skin around the IV needle.
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
Bone modulating drugs
[view] =>Bone modulating drugs
) ) [field_related_products] => Array ( [0] => Array ( [nid] => [i18nsync] => 1 [safe] => Array ( ) [view] => ) [1] => Array ( [nid] => [i18nsync] => 1 [safe] => Array ( ) [view] => ) [2] => Array ( [nid] => [i18nsync] => 1 [safe] => Array ( ) [view] => ) ) [taxonomy] => Array ( [5] => stdClass Object ( [tid] => 5 [vid] => 1 [name] => Hormonal Drugs [description] => [weight] => 3 [language] => [trid] => 0 [v_weight_unused] => 0 ) ) [build_mode] => 0 [readmore] => 1 [content] => Array ( [field_one_image] => Array ( [#type_name] => product [#context] => full [#field_name] => field_one_image [#post_render] => Array ( [0] => content_field_wrapper_post_render ) [#weight] => -3 [field] => Array ( [#description] => [items] => Array ( [0] => Array ( [#formatter] => image_plain [#node] => stdClass Object *RECURSION* [#type_name] => product [#field_name] => field_one_image [#weight] => 0 [#theme] => imagefield_formatter_image_plain [#item] => Array ( [fid] => 237 [uid] => 1 [filename] => pamidronate_s.jpg [filepath] => sites/default/files/images/pamidronate_s.jpg [filemime] => image/jpeg [filesize] => 46889 [status] => 1 [timestamp] => 1329504106 [list] => 1 [data] => Array ( [alt] => [title] => ) [i18nsync] => 1 [nid] => 264 [#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] => )
[#title] =>
[#description] =>
[#children] =>
)
[#title] =>
[#description] =>
[#children] =>  [#printed] => 1
)
[#single] => 1
[#attributes] => Array
(
)
[#required] =>
[#parents] => Array
(
)
[#tree] =>
[#context] => full
[#page] => 1
[#field_name] => field_one_image
[#title] => Image
[#access] => 1
[#label_display] => above
[#teaser] =>
[#node] => stdClass Object
*RECURSION*
[#type] => content_field
[#children] =>
[#printed] => 1
)
[#single] => 1
[#attributes] => Array
(
)
[#required] =>
[#parents] => Array
(
)
[#tree] =>
[#context] => full
[#page] => 1
[#field_name] => field_one_image
[#title] => Image
[#access] => 1
[#label_display] => above
[#teaser] =>
[#node] => stdClass Object
*RECURSION*
[#type] => content_field
[#children] =>  [#printed] => 1
)
[#title] =>
[#description] =>
[#children] =>
[#printed] => 1
)
[#title] =>
[#description] =>
[#children] => 
PAMIDATE®
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>PAMIDATE®
) [#title] => [#description] => [#children] =>PAMIDATE®
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_brand_name [#title] => Brand Name [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>PAMIDATE®
[#printed] => 1 ) [#title] => [#description] => [#children] =>PAMIDATE®
Injection 90mg/10ml
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Injection 90mg/10ml
) [#title] => [#description] => [#children] =>Injection 90mg/10ml
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_dosage_form [#title] => Dosage Form [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Injection 90mg/10ml
[#printed] => 1 ) [#title] => [#description] => [#children] =>Injection 90mg/10ml
Bisphosphonates
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Bisphosphonates
) [#title] => [#description] => [#children] =>Bisphosphonates
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_pharmacological_category [#title] => Pharmacological Category [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Bisphosphonates
[#printed] => 1 ) [#title] => [#description] => [#children] =>Bisphosphonates
Bone modulating drugs
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Bone modulating drugs
) [#title] => [#description] => [#children] =>Bone modulating drugs
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_therapeutic_category [#title] => Therapeutic Category [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Bone modulating drugs
[#printed] => 1 ) [#title] => [#description] => [#children] =>Bone modulating drugs
Category D
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Category D
) [#title] => [#description] => [#children] =>Category D
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_pregnancy_category [#title] => Pregnancy Category [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Category D
[#printed] => 1 ) [#title] => [#description] => [#children] =>Category D
The principal pharmacologic action of Pamidronate disodium is inhibition of bone resorption. Although the mechanism of antiresorptive action is not completely understood, several factors are thought to contribute to this action. Pamidronate disodium adsorbs to calcium phosphate (hydroxyapatite) crystals in bone and may directly block dissolution of this mineral component of bone. In vitro studies also suggest that inhibition of osteoclast activity contributes to inhibition of bone resorption. In animal studies, at doses recommended for the treatment of hypercalcemia, Pamidronate disodium inhibits bone resorption apparently without inhibiting bone formation and mineralization. Of relevance to the treatment of hypercalcemia of malignancy is the finding that Pamidronate disodium inhibits the accelerated bone resorption that results from osteoclast hyperactivity induced by various tumors in animal studies.
[#title] => [#description] => [#printed] => 1 ) [field_pharmacokinetics] => Array ( [#type_name] => product [#context] => full [#field_name] => field_pharmacokinetics [#post_render] => Array ( [0] => content_field_wrapper_post_render ) [#weight] => 4 [field] => Array ( [#description] => [items] => Array ( [0] => Array ( [#formatter] => default [#node] => stdClass Object *RECURSION* [#type_name] => product [#field_name] => field_pharmacokinetics [#weight] => 0 [#theme] => text_formatter_default [#item] => Array ( [value] =>Distribution
The mean ± SD body retention of Pamidronate was calculated to be 54 ± 16% of the dose over 120 hours.
Metabolism
Pamidronate is not metabolized and is exclusively eliminated by renal excretion.
Excretion
After administration of 30, 60, and 90 mg of Pamidronate disodium over 4 hours, and 90 mg of Pamidronate disodium over 24 hours, an overall mean ± SD of 46 ± 16% of the drug was excreted unchanged in the urine within 120 hours. Cumulative urinary excretion was linearly related to dose. The mean ± SD elimination half-life is 28 ± 7 hours. Mean ± SD total and renal clearances of Pamidronate were 107 ± 50 mL/min and 49 ± 28 mL/min, respectively. The rate of elimination from bone has not been determined.
Distribution
The mean ± SD body retention of Pamidronate was calculated to be 54 ± 16% of the dose over 120 hours.
Metabolism
Pamidronate is not metabolized and is exclusively eliminated by renal excretion.
Excretion
After administration of 30, 60, and 90 mg of Pamidronate disodium over 4 hours, and 90 mg of Pamidronate disodium over 24 hours, an overall mean ± SD of 46 ± 16% of the drug was excreted unchanged in the urine within 120 hours. Cumulative urinary excretion was linearly related to dose. The mean ± SD elimination half-life is 28 ± 7 hours. Mean ± SD total and renal clearances of Pamidronate were 107 ± 50 mL/min and 49 ± 28 mL/min, respectively. The rate of elimination from bone has not been determined.
Distribution
The mean ± SD body retention of Pamidronate was calculated to be 54 ± 16% of the dose over 120 hours.
Metabolism
Pamidronate is not metabolized and is exclusively eliminated by renal excretion.
Excretion
After administration of 30, 60, and 90 mg of Pamidronate disodium over 4 hours, and 90 mg of Pamidronate disodium over 24 hours, an overall mean ± SD of 46 ± 16% of the drug was excreted unchanged in the urine within 120 hours. Cumulative urinary excretion was linearly related to dose. The mean ± SD elimination half-life is 28 ± 7 hours. Mean ± SD total and renal clearances of Pamidronate were 107 ± 50 mL/min and 49 ± 28 mL/min, respectively. The rate of elimination from bone has not been determined.
Distribution
The mean ± SD body retention of Pamidronate was calculated to be 54 ± 16% of the dose over 120 hours.
Metabolism
Pamidronate is not metabolized and is exclusively eliminated by renal excretion.
Excretion
After administration of 30, 60, and 90 mg of Pamidronate disodium over 4 hours, and 90 mg of Pamidronate disodium over 24 hours, an overall mean ± SD of 46 ± 16% of the drug was excreted unchanged in the urine within 120 hours. Cumulative urinary excretion was linearly related to dose. The mean ± SD elimination half-life is 28 ± 7 hours. Mean ± SD total and renal clearances of Pamidronate were 107 ± 50 mL/min and 49 ± 28 mL/min, respectively. The rate of elimination from bone has not been determined.
Distribution
The mean ± SD body retention of Pamidronate was calculated to be 54 ± 16% of the dose over 120 hours.
Metabolism
Pamidronate is not metabolized and is exclusively eliminated by renal excretion.
Excretion
After administration of 30, 60, and 90 mg of Pamidronate disodium over 4 hours, and 90 mg of Pamidronate disodium over 24 hours, an overall mean ± SD of 46 ± 16% of the drug was excreted unchanged in the urine within 120 hours. Cumulative urinary excretion was linearly related to dose. The mean ± SD elimination half-life is 28 ± 7 hours. Mean ± SD total and renal clearances of Pamidronate were 107 ± 50 mL/min and 49 ± 28 mL/min, respectively. The rate of elimination from bone has not been determined.
Distribution
The mean ± SD body retention of Pamidronate was calculated to be 54 ± 16% of the dose over 120 hours.
Metabolism
Pamidronate is not metabolized and is exclusively eliminated by renal excretion.
Excretion
After administration of 30, 60, and 90 mg of Pamidronate disodium over 4 hours, and 90 mg of Pamidronate disodium over 24 hours, an overall mean ± SD of 46 ± 16% of the drug was excreted unchanged in the urine within 120 hours. Cumulative urinary excretion was linearly related to dose. The mean ± SD elimination half-life is 28 ± 7 hours. Mean ± SD total and renal clearances of Pamidronate were 107 ± 50 mL/min and 49 ± 28 mL/min, respectively. The rate of elimination from bone has not been determined.
Hypercalcemia of Malignancy
Pamidronate disodium, in conjunction with adequate hydration, is indicated for the treatment of moderate or severe hypercalcemia associated with malignancy, with or without bone metastases. Patients who have either epidermoid or non-epidermoid tumors respond to treatment with Pamidronate disodium. Vigorous saline hydration, an integral part of hypercalcemia therapy, should be initiated promptly and an attempt should be made to restore the urine output to about 2 L/day throughout treatment. Mild or asymptomatic hypercalcemia may be treated with conservative measures (i.e., saline hydration, with or without loop diuretics). Patients should be hydrated adequately throughout the treatment, but overhydration, especially in those patients who have cardiac failure, must be avoided. Diuretic therapy should not be employed prior to correction of hypovolemia. The safety and efficacy of Pamidronate disodium in the treatment of hypercalcemia associated with hyperparathyroidism or with other non-tumor-related conditions has not been established.
Paget's Disease
Pamidronate disodium is indicated for the treatment of patients with moderate to severe Paget's disease of bone. The effectiveness of Pamidronate disodium was demonstrated primarily in patients with serum alkaline phosphatase ≥3 times the upper limit of normal. Pamidronate disodium therapy in patients with Paget's disease has been effective in reducing serum alkaline phosphatase and urinary hydroxyproline levels by ≥50% in at least 50% of patients, and by ≥30% in at least 80% of patients. Pamidronate disodium therapy has also been effective in reducing these biochemical markers in patients with Paget's disease who failed to respond, or no longer responded to other treatments.
Osteolytic Bone Metastases of Breast Cancer and Osteolytic Lesions of Multiple Myeloma
Pamidronate disodium is indicated, in conjunction with standard antineoplastic therapy, for the treatment of osteolytic bone metastases of breast cancer and osteolytic lesions of multiple myeloma. The Pamidronate disodium treatment effect appeared to be smaller in the study of breast cancer patients receiving hormonal therapy than in the study of those receiving chemotherapy, however, overall evidence of clinical benefit has been demonstrated.
Hypercalcemia of Malignancy
Pamidronate disodium, in conjunction with adequate hydration, is indicated for the treatment of moderate or severe hypercalcemia associated with malignancy, with or without bone metastases. Patients who have either epidermoid or non-epidermoid tumors respond to treatment with Pamidronate disodium. Vigorous saline hydration, an integral part of hypercalcemia therapy, should be initiated promptly and an attempt should be made to restore the urine output to about 2 L/day throughout treatment. Mild or asymptomatic hypercalcemia may be treated with conservative measures (i.e., saline hydration, with or without loop diuretics). Patients should be hydrated adequately throughout the treatment, but overhydration, especially in those patients who have cardiac failure, must be avoided. Diuretic therapy should not be employed prior to correction of hypovolemia. The safety and efficacy of Pamidronate disodium in the treatment of hypercalcemia associated with hyperparathyroidism or with other non-tumor-related conditions has not been established.
Paget's Disease
Pamidronate disodium is indicated for the treatment of patients with moderate to severe Paget's disease of bone. The effectiveness of Pamidronate disodium was demonstrated primarily in patients with serum alkaline phosphatase ≥3 times the upper limit of normal. Pamidronate disodium therapy in patients with Paget's disease has been effective in reducing serum alkaline phosphatase and urinary hydroxyproline levels by ≥50% in at least 50% of patients, and by ≥30% in at least 80% of patients. Pamidronate disodium therapy has also been effective in reducing these biochemical markers in patients with Paget's disease who failed to respond, or no longer responded to other treatments.
Osteolytic Bone Metastases of Breast Cancer and Osteolytic Lesions of Multiple Myeloma
Pamidronate disodium is indicated, in conjunction with standard antineoplastic therapy, for the treatment of osteolytic bone metastases of breast cancer and osteolytic lesions of multiple myeloma. The Pamidronate disodium treatment effect appeared to be smaller in the study of breast cancer patients receiving hormonal therapy than in the study of those receiving chemotherapy, however, overall evidence of clinical benefit has been demonstrated.
Hypercalcemia of Malignancy
Pamidronate disodium, in conjunction with adequate hydration, is indicated for the treatment of moderate or severe hypercalcemia associated with malignancy, with or without bone metastases. Patients who have either epidermoid or non-epidermoid tumors respond to treatment with Pamidronate disodium. Vigorous saline hydration, an integral part of hypercalcemia therapy, should be initiated promptly and an attempt should be made to restore the urine output to about 2 L/day throughout treatment. Mild or asymptomatic hypercalcemia may be treated with conservative measures (i.e., saline hydration, with or without loop diuretics). Patients should be hydrated adequately throughout the treatment, but overhydration, especially in those patients who have cardiac failure, must be avoided. Diuretic therapy should not be employed prior to correction of hypovolemia. The safety and efficacy of Pamidronate disodium in the treatment of hypercalcemia associated with hyperparathyroidism or with other non-tumor-related conditions has not been established.
Paget's Disease
Pamidronate disodium is indicated for the treatment of patients with moderate to severe Paget's disease of bone. The effectiveness of Pamidronate disodium was demonstrated primarily in patients with serum alkaline phosphatase ≥3 times the upper limit of normal. Pamidronate disodium therapy in patients with Paget's disease has been effective in reducing serum alkaline phosphatase and urinary hydroxyproline levels by ≥50% in at least 50% of patients, and by ≥30% in at least 80% of patients. Pamidronate disodium therapy has also been effective in reducing these biochemical markers in patients with Paget's disease who failed to respond, or no longer responded to other treatments.
Osteolytic Bone Metastases of Breast Cancer and Osteolytic Lesions of Multiple Myeloma
Pamidronate disodium is indicated, in conjunction with standard antineoplastic therapy, for the treatment of osteolytic bone metastases of breast cancer and osteolytic lesions of multiple myeloma. The Pamidronate disodium treatment effect appeared to be smaller in the study of breast cancer patients receiving hormonal therapy than in the study of those receiving chemotherapy, however, overall evidence of clinical benefit has been demonstrated.
Hypercalcemia of Malignancy
Pamidronate disodium, in conjunction with adequate hydration, is indicated for the treatment of moderate or severe hypercalcemia associated with malignancy, with or without bone metastases. Patients who have either epidermoid or non-epidermoid tumors respond to treatment with Pamidronate disodium. Vigorous saline hydration, an integral part of hypercalcemia therapy, should be initiated promptly and an attempt should be made to restore the urine output to about 2 L/day throughout treatment. Mild or asymptomatic hypercalcemia may be treated with conservative measures (i.e., saline hydration, with or without loop diuretics). Patients should be hydrated adequately throughout the treatment, but overhydration, especially in those patients who have cardiac failure, must be avoided. Diuretic therapy should not be employed prior to correction of hypovolemia. The safety and efficacy of Pamidronate disodium in the treatment of hypercalcemia associated with hyperparathyroidism or with other non-tumor-related conditions has not been established.
Paget's Disease
Pamidronate disodium is indicated for the treatment of patients with moderate to severe Paget's disease of bone. The effectiveness of Pamidronate disodium was demonstrated primarily in patients with serum alkaline phosphatase ≥3 times the upper limit of normal. Pamidronate disodium therapy in patients with Paget's disease has been effective in reducing serum alkaline phosphatase and urinary hydroxyproline levels by ≥50% in at least 50% of patients, and by ≥30% in at least 80% of patients. Pamidronate disodium therapy has also been effective in reducing these biochemical markers in patients with Paget's disease who failed to respond, or no longer responded to other treatments.
Osteolytic Bone Metastases of Breast Cancer and Osteolytic Lesions of Multiple Myeloma
Pamidronate disodium is indicated, in conjunction with standard antineoplastic therapy, for the treatment of osteolytic bone metastases of breast cancer and osteolytic lesions of multiple myeloma. The Pamidronate disodium treatment effect appeared to be smaller in the study of breast cancer patients receiving hormonal therapy than in the study of those receiving chemotherapy, however, overall evidence of clinical benefit has been demonstrated.
Hypercalcemia of Malignancy
Pamidronate disodium, in conjunction with adequate hydration, is indicated for the treatment of moderate or severe hypercalcemia associated with malignancy, with or without bone metastases. Patients who have either epidermoid or non-epidermoid tumors respond to treatment with Pamidronate disodium. Vigorous saline hydration, an integral part of hypercalcemia therapy, should be initiated promptly and an attempt should be made to restore the urine output to about 2 L/day throughout treatment. Mild or asymptomatic hypercalcemia may be treated with conservative measures (i.e., saline hydration, with or without loop diuretics). Patients should be hydrated adequately throughout the treatment, but overhydration, especially in those patients who have cardiac failure, must be avoided. Diuretic therapy should not be employed prior to correction of hypovolemia. The safety and efficacy of Pamidronate disodium in the treatment of hypercalcemia associated with hyperparathyroidism or with other non-tumor-related conditions has not been established.
Paget's Disease
Pamidronate disodium is indicated for the treatment of patients with moderate to severe Paget's disease of bone. The effectiveness of Pamidronate disodium was demonstrated primarily in patients with serum alkaline phosphatase ≥3 times the upper limit of normal. Pamidronate disodium therapy in patients with Paget's disease has been effective in reducing serum alkaline phosphatase and urinary hydroxyproline levels by ≥50% in at least 50% of patients, and by ≥30% in at least 80% of patients. Pamidronate disodium therapy has also been effective in reducing these biochemical markers in patients with Paget's disease who failed to respond, or no longer responded to other treatments.
Osteolytic Bone Metastases of Breast Cancer and Osteolytic Lesions of Multiple Myeloma
Pamidronate disodium is indicated, in conjunction with standard antineoplastic therapy, for the treatment of osteolytic bone metastases of breast cancer and osteolytic lesions of multiple myeloma. The Pamidronate disodium treatment effect appeared to be smaller in the study of breast cancer patients receiving hormonal therapy than in the study of those receiving chemotherapy, however, overall evidence of clinical benefit has been demonstrated.
Hypercalcemia of Malignancy
Pamidronate disodium, in conjunction with adequate hydration, is indicated for the treatment of moderate or severe hypercalcemia associated with malignancy, with or without bone metastases. Patients who have either epidermoid or non-epidermoid tumors respond to treatment with Pamidronate disodium. Vigorous saline hydration, an integral part of hypercalcemia therapy, should be initiated promptly and an attempt should be made to restore the urine output to about 2 L/day throughout treatment. Mild or asymptomatic hypercalcemia may be treated with conservative measures (i.e., saline hydration, with or without loop diuretics). Patients should be hydrated adequately throughout the treatment, but overhydration, especially in those patients who have cardiac failure, must be avoided. Diuretic therapy should not be employed prior to correction of hypovolemia. The safety and efficacy of Pamidronate disodium in the treatment of hypercalcemia associated with hyperparathyroidism or with other non-tumor-related conditions has not been established.
Paget's Disease
Pamidronate disodium is indicated for the treatment of patients with moderate to severe Paget's disease of bone. The effectiveness of Pamidronate disodium was demonstrated primarily in patients with serum alkaline phosphatase ≥3 times the upper limit of normal. Pamidronate disodium therapy in patients with Paget's disease has been effective in reducing serum alkaline phosphatase and urinary hydroxyproline levels by ≥50% in at least 50% of patients, and by ≥30% in at least 80% of patients. Pamidronate disodium therapy has also been effective in reducing these biochemical markers in patients with Paget's disease who failed to respond, or no longer responded to other treatments.
Osteolytic Bone Metastases of Breast Cancer and Osteolytic Lesions of Multiple Myeloma
Pamidronate disodium is indicated, in conjunction with standard antineoplastic therapy, for the treatment of osteolytic bone metastases of breast cancer and osteolytic lesions of multiple myeloma. The Pamidronate disodium treatment effect appeared to be smaller in the study of breast cancer patients receiving hormonal therapy than in the study of those receiving chemotherapy, however, overall evidence of clinical benefit has been demonstrated.
Pamidronate disodium is contraindicated in patients with clinically significant hypersensitivity to Pamidronate disodium or other bisphosphonates.
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Pamidronate disodium is contraindicated in patients with clinically significant hypersensitivity to Pamidronate disodium or other bisphosphonates.
) [#title] => [#description] => [#children] =>Pamidronate disodium is contraindicated in patients with clinically significant hypersensitivity to Pamidronate disodium or other bisphosphonates.
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_contraindications [#title] => Contraindications [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Pamidronate disodium is contraindicated in patients with clinically significant hypersensitivity to Pamidronate disodium or other bisphosphonates.
[#printed] => 1 ) [#title] => [#description] => [#children] =>Pamidronate disodium is contraindicated in patients with clinically significant hypersensitivity to Pamidronate disodium or other bisphosphonates.
Standard hypercalcemia-related metabolic parameters, such as serum levels of calcium, phosphate, magnesium, and potassium, should be carefully monitored following initiation of therapy with Pamidronate disodium. Cases of asymptomatic hypophosphatemia (12%), hypokalemia (7%), hypomagnesemia (11%), and hypocalcemia (5% to 12%), were reported in Pamidronate disodium-treated patients. Rare cases of symptomatic hypocalcemia (including tetany) have been reported in association with Pamidronate therapy. If hypocalcemia occurs, short-term calcium therapy may be necessary. In Paget's disease of bone, 17% of patients treated with 90 mg of Pamidronate disodium showed serum calcium levels below 8 mg/dL.
Patients with a history of thyroid surgery may have relative hypoparathyroidism that may predispose to hypocalcemia with Pamidronate disodium.
Renal Insufficiency
Pamidronate disodium is excreted intact primarily via the kidney, and the risk of renal adverse reactions may be greater in patients with impaired renal function. Patients who receive Pamidronate disodium should have serum creatinine assessed prior to each treatment. In patients receiving Pamidronate disodium for bone metastases, who show evidence of deterioration in renal function, Pamidronate disodium treatment should be withheld until renal function returns to baseline.
In clinical trials, patients with renal impairment (serum creatinine >3.0 mg/dL) have not been studied. Limited pharmacokinetic data exist in patients with creatinine clearance <30 mL/min For the treatment of bone metastases, the use of Pamidronate disodium in patients with severe renal impairment is not recommended. In other indications, clinical judgement should determine whether the potential benefit outweighs the potential risk in such patients.
Osteonecrosis of the Jaw
Osteonecrosis of the jaw (ONJ) has been reported predominantly in cancer patients treated with intravenous biphosphonates, including Pamidronate disodium. Many of these patients were also receiving chemotherapy and corticosteroids which may be risk factors for ONJ. Postmarketing experience and the literature suggests a greater frequency of reports of ONJ based on tumor type (advanced breast cancer, multiple myeloma), and dental status (dental extraction, periodontal disease, local trauma including poorly fitting dentures). Many reports of ONJ involved patients with signs of local infection including osteomyelitis.
Cancer patients should maintain good oral hygiene and should have a dental examination with preventive dentistry prior to treatment with bisphophonates.
While on treatment, these patients should avoid invasive dental procedures if possible. For patients who develop ONJ while on bisphosphonate therapy, dental surgery may exacerbate the condition. For patients requiring dental procedures, there are no data available to suggest whether discontinuation of bisphosphonate treatment reduces the risk of ONJ. Clinical judgement of the treating physician should guide the management plan of each patient based on individual benefit/risk assessment.
Standard hypercalcemia-related metabolic parameters, such as serum levels of calcium, phosphate, magnesium, and potassium, should be carefully monitored following initiation of therapy with Pamidronate disodium. Cases of asymptomatic hypophosphatemia (12%), hypokalemia (7%), hypomagnesemia (11%), and hypocalcemia (5% to 12%), were reported in Pamidronate disodium-treated patients. Rare cases of symptomatic hypocalcemia (including tetany) have been reported in association with Pamidronate therapy. If hypocalcemia occurs, short-term calcium therapy may be necessary. In Paget's disease of bone, 17% of patients treated with 90 mg of Pamidronate disodium showed serum calcium levels below 8 mg/dL.
Patients with a history of thyroid surgery may have relative hypoparathyroidism that may predispose to hypocalcemia with Pamidronate disodium.
Renal Insufficiency
Pamidronate disodium is excreted intact primarily via the kidney, and the risk of renal adverse reactions may be greater in patients with impaired renal function. Patients who receive Pamidronate disodium should have serum creatinine assessed prior to each treatment. In patients receiving Pamidronate disodium for bone metastases, who show evidence of deterioration in renal function, Pamidronate disodium treatment should be withheld until renal function returns to baseline.
In clinical trials, patients with renal impairment (serum creatinine >3.0 mg/dL) have not been studied. Limited pharmacokinetic data exist in patients with creatinine clearance <30 mL/min For the treatment of bone metastases, the use of Pamidronate disodium in patients with severe renal impairment is not recommended. In other indications, clinical judgement should determine whether the potential benefit outweighs the potential risk in such patients.
Osteonecrosis of the Jaw
Osteonecrosis of the jaw (ONJ) has been reported predominantly in cancer patients treated with intravenous biphosphonates, including Pamidronate disodium. Many of these patients were also receiving chemotherapy and corticosteroids which may be risk factors for ONJ. Postmarketing experience and the literature suggests a greater frequency of reports of ONJ based on tumor type (advanced breast cancer, multiple myeloma), and dental status (dental extraction, periodontal disease, local trauma including poorly fitting dentures). Many reports of ONJ involved patients with signs of local infection including osteomyelitis.
Cancer patients should maintain good oral hygiene and should have a dental examination with preventive dentistry prior to treatment with bisphophonates.
While on treatment, these patients should avoid invasive dental procedures if possible. For patients who develop ONJ while on bisphosphonate therapy, dental surgery may exacerbate the condition. For patients requiring dental procedures, there are no data available to suggest whether discontinuation of bisphosphonate treatment reduces the risk of ONJ. Clinical judgement of the treating physician should guide the management plan of each patient based on individual benefit/risk assessment.
Standard hypercalcemia-related metabolic parameters, such as serum levels of calcium, phosphate, magnesium, and potassium, should be carefully monitored following initiation of therapy with Pamidronate disodium. Cases of asymptomatic hypophosphatemia (12%), hypokalemia (7%), hypomagnesemia (11%), and hypocalcemia (5% to 12%), were reported in Pamidronate disodium-treated patients. Rare cases of symptomatic hypocalcemia (including tetany) have been reported in association with Pamidronate therapy. If hypocalcemia occurs, short-term calcium therapy may be necessary. In Paget's disease of bone, 17% of patients treated with 90 mg of Pamidronate disodium showed serum calcium levels below 8 mg/dL.
Patients with a history of thyroid surgery may have relative hypoparathyroidism that may predispose to hypocalcemia with Pamidronate disodium.
Renal Insufficiency
Pamidronate disodium is excreted intact primarily via the kidney, and the risk of renal adverse reactions may be greater in patients with impaired renal function. Patients who receive Pamidronate disodium should have serum creatinine assessed prior to each treatment. In patients receiving Pamidronate disodium for bone metastases, who show evidence of deterioration in renal function, Pamidronate disodium treatment should be withheld until renal function returns to baseline.
In clinical trials, patients with renal impairment (serum creatinine >3.0 mg/dL) have not been studied. Limited pharmacokinetic data exist in patients with creatinine clearance <30 mL/min For the treatment of bone metastases, the use of Pamidronate disodium in patients with severe renal impairment is not recommended. In other indications, clinical judgement should determine whether the potential benefit outweighs the potential risk in such patients.
Osteonecrosis of the Jaw
Osteonecrosis of the jaw (ONJ) has been reported predominantly in cancer patients treated with intravenous biphosphonates, including Pamidronate disodium. Many of these patients were also receiving chemotherapy and corticosteroids which may be risk factors for ONJ. Postmarketing experience and the literature suggests a greater frequency of reports of ONJ based on tumor type (advanced breast cancer, multiple myeloma), and dental status (dental extraction, periodontal disease, local trauma including poorly fitting dentures). Many reports of ONJ involved patients with signs of local infection including osteomyelitis.
Cancer patients should maintain good oral hygiene and should have a dental examination with preventive dentistry prior to treatment with bisphophonates.
While on treatment, these patients should avoid invasive dental procedures if possible. For patients who develop ONJ while on bisphosphonate therapy, dental surgery may exacerbate the condition. For patients requiring dental procedures, there are no data available to suggest whether discontinuation of bisphosphonate treatment reduces the risk of ONJ. Clinical judgement of the treating physician should guide the management plan of each patient based on individual benefit/risk assessment.
Standard hypercalcemia-related metabolic parameters, such as serum levels of calcium, phosphate, magnesium, and potassium, should be carefully monitored following initiation of therapy with Pamidronate disodium. Cases of asymptomatic hypophosphatemia (12%), hypokalemia (7%), hypomagnesemia (11%), and hypocalcemia (5% to 12%), were reported in Pamidronate disodium-treated patients. Rare cases of symptomatic hypocalcemia (including tetany) have been reported in association with Pamidronate therapy. If hypocalcemia occurs, short-term calcium therapy may be necessary. In Paget's disease of bone, 17% of patients treated with 90 mg of Pamidronate disodium showed serum calcium levels below 8 mg/dL.
Patients with a history of thyroid surgery may have relative hypoparathyroidism that may predispose to hypocalcemia with Pamidronate disodium.
Renal Insufficiency
Pamidronate disodium is excreted intact primarily via the kidney, and the risk of renal adverse reactions may be greater in patients with impaired renal function. Patients who receive Pamidronate disodium should have serum creatinine assessed prior to each treatment. In patients receiving Pamidronate disodium for bone metastases, who show evidence of deterioration in renal function, Pamidronate disodium treatment should be withheld until renal function returns to baseline.
In clinical trials, patients with renal impairment (serum creatinine >3.0 mg/dL) have not been studied. Limited pharmacokinetic data exist in patients with creatinine clearance <30 mL/min For the treatment of bone metastases, the use of Pamidronate disodium in patients with severe renal impairment is not recommended. In other indications, clinical judgement should determine whether the potential benefit outweighs the potential risk in such patients.
Osteonecrosis of the Jaw
Osteonecrosis of the jaw (ONJ) has been reported predominantly in cancer patients treated with intravenous biphosphonates, including Pamidronate disodium. Many of these patients were also receiving chemotherapy and corticosteroids which may be risk factors for ONJ. Postmarketing experience and the literature suggests a greater frequency of reports of ONJ based on tumor type (advanced breast cancer, multiple myeloma), and dental status (dental extraction, periodontal disease, local trauma including poorly fitting dentures). Many reports of ONJ involved patients with signs of local infection including osteomyelitis.
Cancer patients should maintain good oral hygiene and should have a dental examination with preventive dentistry prior to treatment with bisphophonates.
While on treatment, these patients should avoid invasive dental procedures if possible. For patients who develop ONJ while on bisphosphonate therapy, dental surgery may exacerbate the condition. For patients requiring dental procedures, there are no data available to suggest whether discontinuation of bisphosphonate treatment reduces the risk of ONJ. Clinical judgement of the treating physician should guide the management plan of each patient based on individual benefit/risk assessment.
Standard hypercalcemia-related metabolic parameters, such as serum levels of calcium, phosphate, magnesium, and potassium, should be carefully monitored following initiation of therapy with Pamidronate disodium. Cases of asymptomatic hypophosphatemia (12%), hypokalemia (7%), hypomagnesemia (11%), and hypocalcemia (5% to 12%), were reported in Pamidronate disodium-treated patients. Rare cases of symptomatic hypocalcemia (including tetany) have been reported in association with Pamidronate therapy. If hypocalcemia occurs, short-term calcium therapy may be necessary. In Paget's disease of bone, 17% of patients treated with 90 mg of Pamidronate disodium showed serum calcium levels below 8 mg/dL.
Patients with a history of thyroid surgery may have relative hypoparathyroidism that may predispose to hypocalcemia with Pamidronate disodium.
Renal Insufficiency
Pamidronate disodium is excreted intact primarily via the kidney, and the risk of renal adverse reactions may be greater in patients with impaired renal function. Patients who receive Pamidronate disodium should have serum creatinine assessed prior to each treatment. In patients receiving Pamidronate disodium for bone metastases, who show evidence of deterioration in renal function, Pamidronate disodium treatment should be withheld until renal function returns to baseline.
In clinical trials, patients with renal impairment (serum creatinine >3.0 mg/dL) have not been studied. Limited pharmacokinetic data exist in patients with creatinine clearance <30 mL/min For the treatment of bone metastases, the use of Pamidronate disodium in patients with severe renal impairment is not recommended. In other indications, clinical judgement should determine whether the potential benefit outweighs the potential risk in such patients.
Osteonecrosis of the Jaw
Osteonecrosis of the jaw (ONJ) has been reported predominantly in cancer patients treated with intravenous biphosphonates, including Pamidronate disodium. Many of these patients were also receiving chemotherapy and corticosteroids which may be risk factors for ONJ. Postmarketing experience and the literature suggests a greater frequency of reports of ONJ based on tumor type (advanced breast cancer, multiple myeloma), and dental status (dental extraction, periodontal disease, local trauma including poorly fitting dentures). Many reports of ONJ involved patients with signs of local infection including osteomyelitis.
Cancer patients should maintain good oral hygiene and should have a dental examination with preventive dentistry prior to treatment with bisphophonates.
While on treatment, these patients should avoid invasive dental procedures if possible. For patients who develop ONJ while on bisphosphonate therapy, dental surgery may exacerbate the condition. For patients requiring dental procedures, there are no data available to suggest whether discontinuation of bisphosphonate treatment reduces the risk of ONJ. Clinical judgement of the treating physician should guide the management plan of each patient based on individual benefit/risk assessment.
Standard hypercalcemia-related metabolic parameters, such as serum levels of calcium, phosphate, magnesium, and potassium, should be carefully monitored following initiation of therapy with Pamidronate disodium. Cases of asymptomatic hypophosphatemia (12%), hypokalemia (7%), hypomagnesemia (11%), and hypocalcemia (5% to 12%), were reported in Pamidronate disodium-treated patients. Rare cases of symptomatic hypocalcemia (including tetany) have been reported in association with Pamidronate therapy. If hypocalcemia occurs, short-term calcium therapy may be necessary. In Paget's disease of bone, 17% of patients treated with 90 mg of Pamidronate disodium showed serum calcium levels below 8 mg/dL.
Patients with a history of thyroid surgery may have relative hypoparathyroidism that may predispose to hypocalcemia with Pamidronate disodium.
Renal Insufficiency
Pamidronate disodium is excreted intact primarily via the kidney, and the risk of renal adverse reactions may be greater in patients with impaired renal function. Patients who receive Pamidronate disodium should have serum creatinine assessed prior to each treatment. In patients receiving Pamidronate disodium for bone metastases, who show evidence of deterioration in renal function, Pamidronate disodium treatment should be withheld until renal function returns to baseline.
In clinical trials, patients with renal impairment (serum creatinine >3.0 mg/dL) have not been studied. Limited pharmacokinetic data exist in patients with creatinine clearance <30 mL/min For the treatment of bone metastases, the use of Pamidronate disodium in patients with severe renal impairment is not recommended. In other indications, clinical judgement should determine whether the potential benefit outweighs the potential risk in such patients.
Osteonecrosis of the Jaw
Osteonecrosis of the jaw (ONJ) has been reported predominantly in cancer patients treated with intravenous biphosphonates, including Pamidronate disodium. Many of these patients were also receiving chemotherapy and corticosteroids which may be risk factors for ONJ. Postmarketing experience and the literature suggests a greater frequency of reports of ONJ based on tumor type (advanced breast cancer, multiple myeloma), and dental status (dental extraction, periodontal disease, local trauma including poorly fitting dentures). Many reports of ONJ involved patients with signs of local infection including osteomyelitis.
Cancer patients should maintain good oral hygiene and should have a dental examination with preventive dentistry prior to treatment with bisphophonates.
While on treatment, these patients should avoid invasive dental procedures if possible. For patients who develop ONJ while on bisphosphonate therapy, dental surgery may exacerbate the condition. For patients requiring dental procedures, there are no data available to suggest whether discontinuation of bisphosphonate treatment reduces the risk of ONJ. Clinical judgement of the treating physician should guide the management plan of each patient based on individual benefit/risk assessment.
Pamidronate can harm your kidneys. This effect is increased when you also use other medicines harmful to the kidneys. You may need dose adjustments or special tests if you have recently used:
• lithium
• methotrexate
• pain or arthritis medicines such as aspirin, acetaminophen, diclofenac, etodolac , ibuprofen, indomethacin, naproxen, and others
• medicines used to treat ulcerative colitis, such as mesalamine (Pentasa) or sulfasalazine
• medicines used to prevent organ transplant rejection, such as cyclosporine (Neoral, Sandimmune), sirolimus (Rapamune) or tacrolimus (Prograf)
• IV antibiotics such as amphotericin B (Fungizone), amikacin, bacitracin, capreomycin, gentamicin, kanamycin, streptomycin, or vancomycin
• antiviral medicines such as adefovir (Hepsera), cidofovir, or foscarnet (Foscavir); or
• cancer medicine such as aldesleukin, carmustine (BiCNU), cisplatin, ifosfamide, oxaliplatin (Eloxatin), streptozocin, or tretinoin
Pamidronate can harm your kidneys. This effect is increased when you also use other medicines harmful to the kidneys. You may need dose adjustments or special tests if you have recently used:
• lithium
• methotrexate
• pain or arthritis medicines such as aspirin, acetaminophen, diclofenac, etodolac , ibuprofen, indomethacin, naproxen, and others
• medicines used to treat ulcerative colitis, such as mesalamine (Pentasa) or sulfasalazine
• medicines used to prevent organ transplant rejection, such as cyclosporine (Neoral, Sandimmune), sirolimus (Rapamune) or tacrolimus (Prograf)
• IV antibiotics such as amphotericin B (Fungizone), amikacin, bacitracin, capreomycin, gentamicin, kanamycin, streptomycin, or vancomycin
• antiviral medicines such as adefovir (Hepsera), cidofovir, or foscarnet (Foscavir); or
• cancer medicine such as aldesleukin, carmustine (BiCNU), cisplatin, ifosfamide, oxaliplatin (Eloxatin), streptozocin, or tretinoin
Pamidronate can harm your kidneys. This effect is increased when you also use other medicines harmful to the kidneys. You may need dose adjustments or special tests if you have recently used:
• lithium
• methotrexate
• pain or arthritis medicines such as aspirin, acetaminophen, diclofenac, etodolac , ibuprofen, indomethacin, naproxen, and others
• medicines used to treat ulcerative colitis, such as mesalamine (Pentasa) or sulfasalazine
• medicines used to prevent organ transplant rejection, such as cyclosporine (Neoral, Sandimmune), sirolimus (Rapamune) or tacrolimus (Prograf)
• IV antibiotics such as amphotericin B (Fungizone), amikacin, bacitracin, capreomycin, gentamicin, kanamycin, streptomycin, or vancomycin
• antiviral medicines such as adefovir (Hepsera), cidofovir, or foscarnet (Foscavir); or
• cancer medicine such as aldesleukin, carmustine (BiCNU), cisplatin, ifosfamide, oxaliplatin (Eloxatin), streptozocin, or tretinoin
Pamidronate can harm your kidneys. This effect is increased when you also use other medicines harmful to the kidneys. You may need dose adjustments or special tests if you have recently used:
• lithium
• methotrexate
• pain or arthritis medicines such as aspirin, acetaminophen, diclofenac, etodolac , ibuprofen, indomethacin, naproxen, and others
• medicines used to treat ulcerative colitis, such as mesalamine (Pentasa) or sulfasalazine
• medicines used to prevent organ transplant rejection, such as cyclosporine (Neoral, Sandimmune), sirolimus (Rapamune) or tacrolimus (Prograf)
• IV antibiotics such as amphotericin B (Fungizone), amikacin, bacitracin, capreomycin, gentamicin, kanamycin, streptomycin, or vancomycin
• antiviral medicines such as adefovir (Hepsera), cidofovir, or foscarnet (Foscavir); or
• cancer medicine such as aldesleukin, carmustine (BiCNU), cisplatin, ifosfamide, oxaliplatin (Eloxatin), streptozocin, or tretinoin
Pamidronate can harm your kidneys. This effect is increased when you also use other medicines harmful to the kidneys. You may need dose adjustments or special tests if you have recently used:
• lithium
• methotrexate
• pain or arthritis medicines such as aspirin, acetaminophen, diclofenac, etodolac , ibuprofen, indomethacin, naproxen, and others
• medicines used to treat ulcerative colitis, such as mesalamine (Pentasa) or sulfasalazine
• medicines used to prevent organ transplant rejection, such as cyclosporine (Neoral, Sandimmune), sirolimus (Rapamune) or tacrolimus (Prograf)
• IV antibiotics such as amphotericin B (Fungizone), amikacin, bacitracin, capreomycin, gentamicin, kanamycin, streptomycin, or vancomycin
• antiviral medicines such as adefovir (Hepsera), cidofovir, or foscarnet (Foscavir); or
• cancer medicine such as aldesleukin, carmustine (BiCNU), cisplatin, ifosfamide, oxaliplatin (Eloxatin), streptozocin, or tretinoin
• high fever;
• severe joint, bone, or muscle pain;
• new or unusual pain in your thigh or hip;
• urinating less than usual or not at all;
• swelling, rapid weight gain;
• pain or burning when you urinate;
• seizure (convulsions);
• eye pain, vision changes;
• pale skin, feeling light-headed or short of breath, rapid heart rate, trouble concentrating; or
• confusion, uneven heart rate, extreme thirst, increased urination, leg discomfort, muscle weakness or limp feeling, or jerking muscle movements.
• low fever;
• stomach pain, loss of appetite, nausea, vomiting;
• constipation; or
• pain, redness, swelling or a hard painful lump under your skin around the IV needle.
• high fever;
• severe joint, bone, or muscle pain;
• new or unusual pain in your thigh or hip;
• urinating less than usual or not at all;
• swelling, rapid weight gain;
• pain or burning when you urinate;
• seizure (convulsions);
• eye pain, vision changes;
• pale skin, feeling light-headed or short of breath, rapid heart rate, trouble concentrating; or
• confusion, uneven heart rate, extreme thirst, increased urination, leg discomfort, muscle weakness or limp feeling, or jerking muscle movements.
• low fever;
• stomach pain, loss of appetite, nausea, vomiting;
• constipation; or
• pain, redness, swelling or a hard painful lump under your skin around the IV needle.
• high fever;
• severe joint, bone, or muscle pain;
• new or unusual pain in your thigh or hip;
• urinating less than usual or not at all;
• swelling, rapid weight gain;
• pain or burning when you urinate;
• seizure (convulsions);
• eye pain, vision changes;
• pale skin, feeling light-headed or short of breath, rapid heart rate, trouble concentrating; or
• confusion, uneven heart rate, extreme thirst, increased urination, leg discomfort, muscle weakness or limp feeling, or jerking muscle movements.
• low fever;
• stomach pain, loss of appetite, nausea, vomiting;
• constipation; or
• pain, redness, swelling or a hard painful lump under your skin around the IV needle.
• high fever;
• severe joint, bone, or muscle pain;
• new or unusual pain in your thigh or hip;
• urinating less than usual or not at all;
• swelling, rapid weight gain;
• pain or burning when you urinate;
• seizure (convulsions);
• eye pain, vision changes;
• pale skin, feeling light-headed or short of breath, rapid heart rate, trouble concentrating; or
• confusion, uneven heart rate, extreme thirst, increased urination, leg discomfort, muscle weakness or limp feeling, or jerking muscle movements.
• low fever;
• stomach pain, loss of appetite, nausea, vomiting;
• constipation; or
• pain, redness, swelling or a hard painful lump under your skin around the IV needle.
• high fever;
• severe joint, bone, or muscle pain;
• new or unusual pain in your thigh or hip;
• urinating less than usual or not at all;
• swelling, rapid weight gain;
• pain or burning when you urinate;
• seizure (convulsions);
• eye pain, vision changes;
• pale skin, feeling light-headed or short of breath, rapid heart rate, trouble concentrating; or
• confusion, uneven heart rate, extreme thirst, increased urination, leg discomfort, muscle weakness or limp feeling, or jerking muscle movements.
• low fever;
• stomach pain, loss of appetite, nausea, vomiting;
• constipation; or
• pain, redness, swelling or a hard painful lump under your skin around the IV needle.
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
• Injection 90mg/10ml: Box of 1Ampoule
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>• Injection 90mg/10ml: Box of 1Ampoule
) [#title] => [#description] => [#children] =>• Injection 90mg/10ml: Box of 1Ampoule
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_packing [#title] => Packing [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>• Injection 90mg/10ml: Box of 1Ampoule
[#printed] => 1 ) [#title] => [#description] => [#children] =>• Injection 90mg/10ml: Box of 1Ampoule
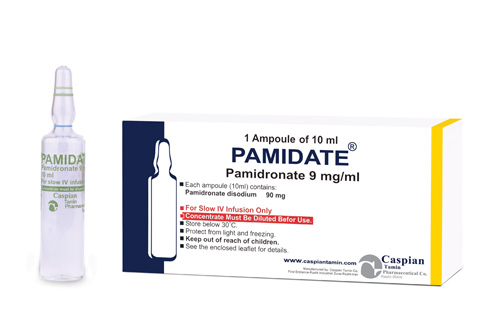
PAMIDATE®
Injection 90mg/10ml
Bisphosphonates
Bone modulating drugs
Category D
The principal pharmacologic action of Pamidronate disodium is inhibition of bone resorption. Although the mechanism of antiresorptive action is not completely understood, several factors are thought to contribute to this action. Pamidronate disodium adsorbs to calcium phosphate (hydroxyapatite) crystals in bone and may directly block dissolution of this mineral component of bone. In vitro studies also suggest that inhibition of osteoclast activity contributes to inhibition of bone resorption. In animal studies, at doses recommended for the treatment of hypercalcemia, Pamidronate disodium inhibits bone resorption apparently without inhibiting bone formation and mineralization. Of relevance to the treatment of hypercalcemia of malignancy is the finding that Pamidronate disodium inhibits the accelerated bone resorption that results from osteoclast hyperactivity induced by various tumors in animal studies.
Distribution
The mean ± SD body retention of Pamidronate was calculated to be 54 ± 16% of the dose over 120 hours.
Metabolism
Pamidronate is not metabolized and is exclusively eliminated by renal excretion.
Excretion
After administration of 30, 60, and 90 mg of Pamidronate disodium over 4 hours, and 90 mg of Pamidronate disodium over 24 hours, an overall mean ± SD of 46 ± 16% of the drug was excreted unchanged in the urine within 120 hours. Cumulative urinary excretion was linearly related to dose. The mean ± SD elimination half-life is 28 ± 7 hours. Mean ± SD total and renal clearances of Pamidronate were 107 ± 50 mL/min and 49 ± 28 mL/min, respectively. The rate of elimination from bone has not been determined.
Hypercalcemia of Malignancy
Pamidronate disodium, in conjunction with adequate hydration, is indicated for the treatment of moderate or severe hypercalcemia associated with malignancy, with or without bone metastases. Patients who have either epidermoid or non-epidermoid tumors respond to treatment with Pamidronate disodium. Vigorous saline hydration, an integral part of hypercalcemia therapy, should be initiated promptly and an attempt should be made to restore the urine output to about 2 L/day throughout treatment. Mild or asymptomatic hypercalcemia may be treated with conservative measures (i.e., saline hydration, with or without loop diuretics). Patients should be hydrated adequately throughout the treatment, but overhydration, especially in those patients who have cardiac failure, must be avoided. Diuretic therapy should not be employed prior to correction of hypovolemia. The safety and efficacy of Pamidronate disodium in the treatment of hypercalcemia associated with hyperparathyroidism or with other non-tumor-related conditions has not been established.
Paget's Disease
Pamidronate disodium is indicated for the treatment of patients with moderate to severe Paget's disease of bone. The effectiveness of Pamidronate disodium was demonstrated primarily in patients with serum alkaline phosphatase ≥3 times the upper limit of normal. Pamidronate disodium therapy in patients with Paget's disease has been effective in reducing serum alkaline phosphatase and urinary hydroxyproline levels by ≥50% in at least 50% of patients, and by ≥30% in at least 80% of patients. Pamidronate disodium therapy has also been effective in reducing these biochemical markers in patients with Paget's disease who failed to respond, or no longer responded to other treatments.
Osteolytic Bone Metastases of Breast Cancer and Osteolytic Lesions of Multiple Myeloma
Pamidronate disodium is indicated, in conjunction with standard antineoplastic therapy, for the treatment of osteolytic bone metastases of breast cancer and osteolytic lesions of multiple myeloma. The Pamidronate disodium treatment effect appeared to be smaller in the study of breast cancer patients receiving hormonal therapy than in the study of those receiving chemotherapy, however, overall evidence of clinical benefit has been demonstrated.
Pamidronate disodium is contraindicated in patients with clinically significant hypersensitivity to Pamidronate disodium or other bisphosphonates.
Standard hypercalcemia-related metabolic parameters, such as serum levels of calcium, phosphate, magnesium, and potassium, should be carefully monitored following initiation of therapy with Pamidronate disodium. Cases of asymptomatic hypophosphatemia (12%), hypokalemia (7%), hypomagnesemia (11%), and hypocalcemia (5% to 12%), were reported in Pamidronate disodium-treated patients. Rare cases of symptomatic hypocalcemia (including tetany) have been reported in association with Pamidronate therapy. If hypocalcemia occurs, short-term calcium therapy may be necessary. In Paget's disease of bone, 17% of patients treated with 90 mg of Pamidronate disodium showed serum calcium levels below 8 mg/dL.
Patients with a history of thyroid surgery may have relative hypoparathyroidism that may predispose to hypocalcemia with Pamidronate disodium.
Renal Insufficiency
Pamidronate disodium is excreted intact primarily via the kidney, and the risk of renal adverse reactions may be greater in patients with impaired renal function. Patients who receive Pamidronate disodium should have serum creatinine assessed prior to each treatment. In patients receiving Pamidronate disodium for bone metastases, who show evidence of deterioration in renal function, Pamidronate disodium treatment should be withheld until renal function returns to baseline.
In clinical trials, patients with renal impairment (serum creatinine >3.0 mg/dL) have not been studied. Limited pharmacokinetic data exist in patients with creatinine clearance <30 mL/min For the treatment of bone metastases, the use of Pamidronate disodium in patients with severe renal impairment is not recommended. In other indications, clinical judgement should determine whether the potential benefit outweighs the potential risk in such patients.
Osteonecrosis of the Jaw
Osteonecrosis of the jaw (ONJ) has been reported predominantly in cancer patients treated with intravenous biphosphonates, including Pamidronate disodium. Many of these patients were also receiving chemotherapy and corticosteroids which may be risk factors for ONJ. Postmarketing experience and the literature suggests a greater frequency of reports of ONJ based on tumor type (advanced breast cancer, multiple myeloma), and dental status (dental extraction, periodontal disease, local trauma including poorly fitting dentures). Many reports of ONJ involved patients with signs of local infection including osteomyelitis.
Cancer patients should maintain good oral hygiene and should have a dental examination with preventive dentistry prior to treatment with bisphophonates.
While on treatment, these patients should avoid invasive dental procedures if possible. For patients who develop ONJ while on bisphosphonate therapy, dental surgery may exacerbate the condition. For patients requiring dental procedures, there are no data available to suggest whether discontinuation of bisphosphonate treatment reduces the risk of ONJ. Clinical judgement of the treating physician should guide the management plan of each patient based on individual benefit/risk assessment.
Pamidronate can harm your kidneys. This effect is increased when you also use other medicines harmful to the kidneys. You may need dose adjustments or special tests if you have recently used:
• lithium
• methotrexate
• pain or arthritis medicines such as aspirin, acetaminophen, diclofenac, etodolac , ibuprofen, indomethacin, naproxen, and others
• medicines used to treat ulcerative colitis, such as mesalamine (Pentasa) or sulfasalazine
• medicines used to prevent organ transplant rejection, such as cyclosporine (Neoral, Sandimmune), sirolimus (Rapamune) or tacrolimus (Prograf)
• IV antibiotics such as amphotericin B (Fungizone), amikacin, bacitracin, capreomycin, gentamicin, kanamycin, streptomycin, or vancomycin
• antiviral medicines such as adefovir (Hepsera), cidofovir, or foscarnet (Foscavir); or
• cancer medicine such as aldesleukin, carmustine (BiCNU), cisplatin, ifosfamide, oxaliplatin (Eloxatin), streptozocin, or tretinoin
• high fever;
• severe joint, bone, or muscle pain;
• new or unusual pain in your thigh or hip;
• urinating less than usual or not at all;
• swelling, rapid weight gain;
• pain or burning when you urinate;
• seizure (convulsions);
• eye pain, vision changes;
• pale skin, feeling light-headed or short of breath, rapid heart rate, trouble concentrating; or
• confusion, uneven heart rate, extreme thirst, increased urination, leg discomfort, muscle weakness or limp feeling, or jerking muscle movements.
• low fever;
• stomach pain, loss of appetite, nausea, vomiting;
• constipation; or
• pain, redness, swelling or a hard painful lump under your skin around the IV needle.
• Store below 30 C°
• Protect from light and freezing
• Injection 90mg/10ml: Box of 1Ampoule