Caspian Products
- Ampoules
- Anlagesics, Anti-inflammatory Drugs
- Antimyasthenics ,Muscle Relaxants
- Antiparkinson Drugs, Antidepressants,Antiepileptics, Anxiolytic Sedative, Hypnotics and Antipsychotics
- Hormonal Drugs
- Antihistamines, Bronchodilators
- Cardiovascular Drugs,Electrolytes
- Corticosteroids
- General Anaesthetics, Local Anaesthetics
- Antibacterials
- Gastrointestinal Drugs
- Nutritional Agents and Vitamins
- Antagonists
- Suppository
- Syrups & Oral Solutions
- Ointments, Creams & Gels
- Vial
- Prefilled Syringe
Haloperidol
Pharmacology
Precise mechanism of antipsychotic action is unclear, but appears to depress the CNS at the subcortical level of the brain, midbrain, and brain stem reticular formation; appears to inhibit the ascending reticular activating system of the brain stem (possibly through the caudate nucleus), thereby interrupting the impulse between the diencephalon and the cortex.
May antagonize actions of glutamic acid within the extrapyramidal system. Inhibition of catecholamine receptors may also be important in the mode of action; may also inhibit the reuptake of various neurotransmitters in the midbrain.
Pharmacokinetics:
Following IM administration of haloperidol lactate, peak plasma haloperidol concentrations occur within 10–20 minutes. Following IM administration of haloperidol lactate, peak pharmacologic action occurs within 30–45 minutes; in acutely agitated patients, control of psychotic manifestations may become apparent within 30–60 minutes, with substantial improvement often occurring within 2–3 hours. Distribution into human body tissues and fluids not fully characterized. In animals, the drug is distributed mainly into the liver, with lower concentrations being distributed into the brain, lungs, kidneys, spleen, and heart. Distributed into milk.
Plasma Protein Binding: About 92%.
Exact metabolic fate not clearly established, but appears to be principally metabolized in the liver by oxidative N-dealkylation of the piperidine nitrogen to form fluorophenylcarbonic acids and piperidine metabolites (which appear to be inactive), and by reduction of the butyrophenone carbonyl to the carbinol, forming hydroxyhaloperidol.
Limited data suggest that the reduced metabolite, hydroxyhaloperidol, has some pharmacologic activity, although its activity appears to be less than that of haloperidol.
Indications:
Haloperidol is used to treat schizophrenia. It is also used to control motor and speech tics in people with Tourette's syndrome.
Contraindications:
• Severe toxic CNS depression or comatose states from any cause.
• Parkinsonian syndrome.
• Hypersensitivity to haloperidol.
Precautions:
Possible risk factors for leukopenia/neutropenia include pre-existing low white blood cell count (WBC) and history of drug-induced leukopenia/neutropenia. Patients with a history of a clinically significant low WBC or a drug-induced leukopenia/neutropenia should have their complete blood count (CBC) monitored frequently during the first few months of therapy and discontinuation of Haloperidol should be considered at the first sign of a clinically significant decline in WBC in the absence of other causative factors.
Patients:
• with clinically significant neutropenia should be carefully monitored for fever or other symptoms or signs of infection and treated promptly if such symptoms or signs occur. Patients with severe neutropenia (absolute neutrophil count < 1000/mm3) should discontinue Haloperidol and have their WBC followed until recovery.
• with severe cardiovascular disorders, because of the possibility of transient hypotension and/or precipitation of anginal pain. Should hypotension occur and a vasopressor be required, epinephrine should not be used since Haloperidol may block its vasopressor activity and paradoxical further lowering of the blood pressure may occur. Instead, metaraminol, phenylephrine or norepinephrine should be used.
• receiving anticonvulsant medications, with a history of seizures, or with EEG abnormalities, because Haloperidol may lower the convulsive threshold. If indicated, adequate anticonvulsant therapy should be concomitantly maintained.
• with known allergies, or with a history of allergic reactions to drugs.
• receiving anticoagulants, since an isolated instance of interference occurred with the effects of one anticoagulant (phenindione).
Drug Interactions:
• arsenic trioxide (Trisenox)
• a blood thinner such as warfarin (Coumadin)
• lithium
• seizure medication
• rifampin
• tacrolimus (Prograf)
• an antibiotic such as clarithromycin (Biaxin), erythromycin ,levofloxacin (Levaquin), moxifloxacin (Avelox), or pentamidine
• an antidepressant such as amitriptylline (Elavil), clomipramine (Anafranil), or desipramine
• anti-malaria medications such as chloroquine or mefloquine
• heart rhythm medicine such as amiodarone (Cordarone), dofetilide, disopyramide, dronedarone, ibutilide, procainamide, propafenone, quinidine, or sotalol
• medicine to prevent or treat nausea and vomiting such as dolasetron (Anzemet), droperidol or ondansetron (Zofran);
• medicines to treat psychiatric disorders, such as chlorpromazine, clozapine, pimozide (Orap), thioridazine (Mellaril), or ziprasidone
• migraine headache medicine such as sumatriptan or zolmitriptan (Zomig); or
• narcotic medication such as methadone
Side Effects:
• dizziness, fainting, fast or pounding heartbeat;
• restless muscle movements in your eyes, tongue, jaw, or neck;
• tremor (uncontrolled shaking);
• seizure (convulsions);
• pale skin, easy bruising or bleeding, flu symptoms;
• very stiff (rigid) muscles, high fever, sweating, confusion, fast or uneven heartbeats, tremors, feeling like you might pass out;
• stabbing chest pain, feeling short of breath, cough with yellow or green mucus;
• sudden mood changes, agitation, hallucinations, unusual thoughts or behavior; or
• jaundice (yellowing of your skin or eyes).
Less serious side effects may include:
• headache, dizziness, spinning sensation, drowsiness;
• sleep problems (insomnia);
• feeling restless or anxious;
• mild skin rash or itching;
• breast enlargement, irregular menstrual periods, loss of interest in sex; or
• dry mouth, blurred vision, urinating less than usual.
Storage:
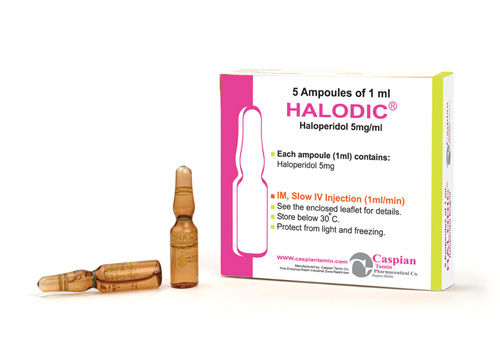
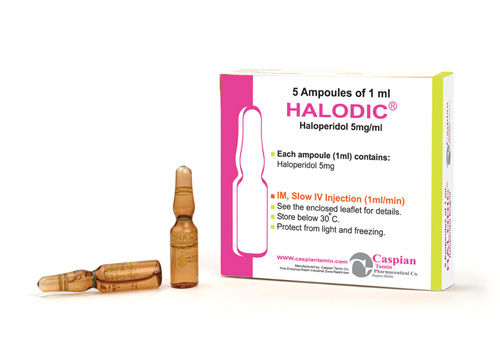
• Store below 30 C°
• Protect from light and freezing
Packing:
• Injection 5mg/1ml: Box of 5 Ampoules
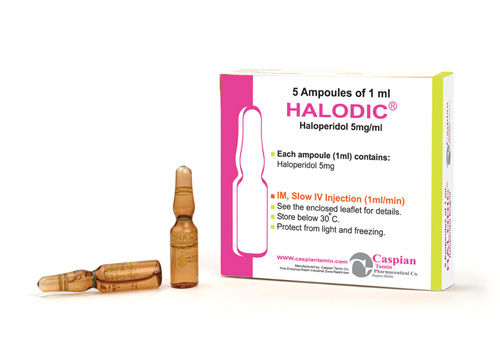
HALODIC®
Injection 5mg/1ml
Butyrophenones
Antipsychotic
category C
Precise mechanism of antipsychotic action is unclear, but appears to depress the CNS at the subcortical level of the brain, midbrain, and brain stem reticular formation; appears to inhibit the ascending reticular activating system of the brain stem (possibly through the caudate nucleus), thereby interrupting the impulse between the diencephalon and the cortex.
May antagonize actions of glutamic acid within the extrapyramidal system. Inhibition of catecholamine receptors may also be important in the mode of action; may also inhibit the reuptake of various neurotransmitters in the midbrain.
Following IM administration of haloperidol lactate, peak plasma haloperidol concentrations occur within 10–20 minutes. Following IM administration of haloperidol lactate, peak pharmacologic action occurs within 30–45 minutes; in acutely agitated patients, control of psychotic manifestations may become apparent within 30–60 minutes, with substantial improvement often occurring within 2–3 hours. Distribution into human body tissues and fluids not fully characterized. In animals, the drug is distributed mainly into the liver, with lower concentrations being distributed into the brain, lungs, kidneys, spleen, and heart. Distributed into milk.
Plasma Protein Binding: About 92%.
Exact metabolic fate not clearly established, but appears to be principally metabolized in the liver by oxidative N-dealkylation of the piperidine nitrogen to form fluorophenylcarbonic acids and piperidine metabolites (which appear to be inactive), and by reduction of the butyrophenone carbonyl to the carbinol, forming hydroxyhaloperidol.
Limited data suggest that the reduced metabolite, hydroxyhaloperidol, has some pharmacologic activity, although its activity appears to be less than that of haloperidol.
Haloperidol is used to treat schizophrenia. It is also used to control motor and speech tics in people with Tourette's syndrome.
• Severe toxic CNS depression or comatose states from any cause.
• Parkinsonian syndrome.
• Hypersensitivity to haloperidol.
Possible risk factors for leukopenia/neutropenia include pre-existing low white blood cell count (WBC) and history of drug-induced leukopenia/neutropenia. Patients with a history of a clinically significant low WBC or a drug-induced leukopenia/neutropenia should have their complete blood count (CBC) monitored frequently during the first few months of therapy and discontinuation of Haloperidol should be considered at the first sign of a clinically significant decline in WBC in the absence of other causative factors.
Patients:
• with clinically significant neutropenia should be carefully monitored for fever or other symptoms or signs of infection and treated promptly if such symptoms or signs occur. Patients with severe neutropenia (absolute neutrophil count < 1000/mm3) should discontinue Haloperidol and have their WBC followed until recovery.
• with severe cardiovascular disorders, because of the possibility of transient hypotension and/or precipitation of anginal pain. Should hypotension occur and a vasopressor be required, epinephrine should not be used since Haloperidol may block its vasopressor activity and paradoxical further lowering of the blood pressure may occur. Instead, metaraminol, phenylephrine or norepinephrine should be used.
• receiving anticonvulsant medications, with a history of seizures, or with EEG abnormalities, because Haloperidol may lower the convulsive threshold. If indicated, adequate anticonvulsant therapy should be concomitantly maintained.
• with known allergies, or with a history of allergic reactions to drugs.
• receiving anticoagulants, since an isolated instance of interference occurred with the effects of one anticoagulant (phenindione).
• arsenic trioxide (Trisenox)
• a blood thinner such as warfarin (Coumadin)
• lithium
• seizure medication
• rifampin
• tacrolimus (Prograf)
• an antibiotic such as clarithromycin (Biaxin), erythromycin ,levofloxacin (Levaquin), moxifloxacin (Avelox), or pentamidine
• an antidepressant such as amitriptylline (Elavil), clomipramine (Anafranil), or desipramine
• anti-malaria medications such as chloroquine or mefloquine
• heart rhythm medicine such as amiodarone (Cordarone), dofetilide, disopyramide, dronedarone, ibutilide, procainamide, propafenone, quinidine, or sotalol
• medicine to prevent or treat nausea and vomiting such as dolasetron (Anzemet), droperidol or ondansetron (Zofran);
• medicines to treat psychiatric disorders, such as chlorpromazine, clozapine, pimozide (Orap), thioridazine (Mellaril), or ziprasidone
• migraine headache medicine such as sumatriptan or zolmitriptan (Zomig); or
• narcotic medication such as methadone
• dizziness, fainting, fast or pounding heartbeat;
• restless muscle movements in your eyes, tongue, jaw, or neck;
• tremor (uncontrolled shaking);
• seizure (convulsions);
• pale skin, easy bruising or bleeding, flu symptoms;
• very stiff (rigid) muscles, high fever, sweating, confusion, fast or uneven heartbeats, tremors, feeling like you might pass out;
• stabbing chest pain, feeling short of breath, cough with yellow or green mucus;
• sudden mood changes, agitation, hallucinations, unusual thoughts or behavior; or
• jaundice (yellowing of your skin or eyes).
Less serious side effects may include:
• headache, dizziness, spinning sensation, drowsiness;
• sleep problems (insomnia);
• feeling restless or anxious;
• mild skin rash or itching;
• breast enlargement, irregular menstrual periods, loss of interest in sex; or
• dry mouth, blurred vision, urinating less than usual.
• Store below 30 C°
• Protect from light and freezing
• Injection 5mg/1ml: Box of 5 Ampoules
 )
)
[field_administration_and_dosage] => Array
(
[0] => Array
(
[value] =>
[format] =>
[safe] =>
[view] =>
)
)
[field_brand_name] => Array
(
[0] => Array
(
[value] => HALODIC®
[format] => 1
[safe] =>
)
)
[field_administration_and_dosage] => Array
(
[0] => Array
(
[value] =>
[format] =>
[safe] =>
[view] =>
)
)
[field_brand_name] => Array
(
[0] => Array
(
[value] => HALODIC®
[format] => 1
[safe] => HALODIC®
[view] =>HALODIC®
) ) [field_contraindications] => Array ( [0] => Array ( [value] => • Severe toxic CNS depression or comatose states from any cause. • Parkinsonian syndrome. • Hypersensitivity to haloperidol. [format] => 1 [safe] =>• Severe toxic CNS depression or comatose states from any cause.
• Parkinsonian syndrome.
• Hypersensitivity to haloperidol.
• Severe toxic CNS depression or comatose states from any cause.
• Parkinsonian syndrome.
• Hypersensitivity to haloperidol.
Injection 5mg/1ml
[view] =>Injection 5mg/1ml
) ) [field_drug_interactions] => Array ( [0] => Array ( [value] => • arsenic trioxide (Trisenox) • a blood thinner such as warfarin (Coumadin) • lithium • seizure medication • rifampin • tacrolimus (Prograf) • an antibiotic such as clarithromycin (Biaxin), erythromycin ,levofloxacin (Levaquin), moxifloxacin (Avelox), or pentamidine • an antidepressant such as amitriptylline (Elavil), clomipramine (Anafranil), or desipramine • anti-malaria medications such as chloroquine or mefloquine • heart rhythm medicine such as amiodarone (Cordarone), dofetilide, disopyramide, dronedarone, ibutilide, procainamide, propafenone, quinidine, or sotalol • medicine to prevent or treat nausea and vomiting such as dolasetron (Anzemet), droperidol or ondansetron (Zofran); • medicines to treat psychiatric disorders, such as chlorpromazine, clozapine, pimozide (Orap), thioridazine (Mellaril), or ziprasidone • migraine headache medicine such as sumatriptan or zolmitriptan (Zomig); or • narcotic medication such as methadone [format] => 1 [safe] =>• arsenic trioxide (Trisenox)
• a blood thinner such as warfarin (Coumadin)
• lithium
• seizure medication
• rifampin
• tacrolimus (Prograf)
• an antibiotic such as clarithromycin (Biaxin), erythromycin ,levofloxacin (Levaquin), moxifloxacin (Avelox), or pentamidine
• an antidepressant such as amitriptylline (Elavil), clomipramine (Anafranil), or desipramine
• anti-malaria medications such as chloroquine or mefloquine
• heart rhythm medicine such as amiodarone (Cordarone), dofetilide, disopyramide, dronedarone, ibutilide, procainamide, propafenone, quinidine, or sotalol
• medicine to prevent or treat nausea and vomiting such as dolasetron (Anzemet), droperidol or ondansetron (Zofran);
• medicines to treat psychiatric disorders, such as chlorpromazine, clozapine, pimozide (Orap), thioridazine (Mellaril), or ziprasidone
• migraine headache medicine such as sumatriptan or zolmitriptan (Zomig); or
• narcotic medication such as methadone
• arsenic trioxide (Trisenox)
• a blood thinner such as warfarin (Coumadin)
• lithium
• seizure medication
• rifampin
• tacrolimus (Prograf)
• an antibiotic such as clarithromycin (Biaxin), erythromycin ,levofloxacin (Levaquin), moxifloxacin (Avelox), or pentamidine
• an antidepressant such as amitriptylline (Elavil), clomipramine (Anafranil), or desipramine
• anti-malaria medications such as chloroquine or mefloquine
• heart rhythm medicine such as amiodarone (Cordarone), dofetilide, disopyramide, dronedarone, ibutilide, procainamide, propafenone, quinidine, or sotalol
• medicine to prevent or treat nausea and vomiting such as dolasetron (Anzemet), droperidol or ondansetron (Zofran);
• medicines to treat psychiatric disorders, such as chlorpromazine, clozapine, pimozide (Orap), thioridazine (Mellaril), or ziprasidone
• migraine headache medicine such as sumatriptan or zolmitriptan (Zomig); or
• narcotic medication such as methadone
Haloperidol is used to treat schizophrenia. It is also used to control motor and speech tics in people with Tourette's syndrome.
[view] =>Haloperidol is used to treat schizophrenia. It is also used to control motor and speech tics in people with Tourette's syndrome.
) ) [field_packing] => Array ( [0] => Array ( [value] => • Injection 5mg/1ml: Box of 5 Ampoules [format] => 1 [safe] =>• Injection 5mg/1ml: Box of 5 Ampoules
[view] =>• Injection 5mg/1ml: Box of 5 Ampoules
) ) [field_pdf] => Array ( [0] => Array ( [fid] => 185 [uid] => 1 [filename] => haloperidol.pdf [filepath] => sites/default/files/pdf/haloperidol.pdf [filemime] => application/pdf [filesize] => 129362 [status] => 1 [timestamp] => 1329489194 [list] => 1 [data] => [i18nsync] => 1 [nid] => 272 [view] => ) ) [field_pharmacokinetics] => Array ( [0] => Array ( [value] => Following IM administration of haloperidol lactate, peak plasma haloperidol concentrations occur within 10–20 minutes. Following IM administration of haloperidol lactate, peak pharmacologic action occurs within 30–45 minutes; in acutely agitated patients, control of psychotic manifestations may become apparent within 30–60 minutes, with substantial improvement often occurring within 2–3 hours. Distribution into human body tissues and fluids not fully characterized. In animals, the drug is distributed mainly into the liver, with lower concentrations being distributed into the brain, lungs, kidneys, spleen, and heart. Distributed into milk. Plasma Protein Binding: About 92%. Exact metabolic fate not clearly established, but appears to be principally metabolized in the liver by oxidative N-dealkylation of the piperidine nitrogen to form fluorophenylcarbonic acids and piperidine metabolites (which appear to be inactive), and by reduction of the butyrophenone carbonyl to the carbinol, forming hydroxyhaloperidol. Limited data suggest that the reduced metabolite, hydroxyhaloperidol, has some pharmacologic activity, although its activity appears to be less than that of haloperidol. [format] => 1 [safe] =>Following IM administration of haloperidol lactate, peak plasma haloperidol concentrations occur within 10–20 minutes. Following IM administration of haloperidol lactate, peak pharmacologic action occurs within 30–45 minutes; in acutely agitated patients, control of psychotic manifestations may become apparent within 30–60 minutes, with substantial improvement often occurring within 2–3 hours. Distribution into human body tissues and fluids not fully characterized. In animals, the drug is distributed mainly into the liver, with lower concentrations being distributed into the brain, lungs, kidneys, spleen, and heart. Distributed into milk.
Plasma Protein Binding: About 92%.
Exact metabolic fate not clearly established, but appears to be principally metabolized in the liver by oxidative N-dealkylation of the piperidine nitrogen to form fluorophenylcarbonic acids and piperidine metabolites (which appear to be inactive), and by reduction of the butyrophenone carbonyl to the carbinol, forming hydroxyhaloperidol.
Limited data suggest that the reduced metabolite, hydroxyhaloperidol, has some pharmacologic activity, although its activity appears to be less than that of haloperidol.
Following IM administration of haloperidol lactate, peak plasma haloperidol concentrations occur within 10–20 minutes. Following IM administration of haloperidol lactate, peak pharmacologic action occurs within 30–45 minutes; in acutely agitated patients, control of psychotic manifestations may become apparent within 30–60 minutes, with substantial improvement often occurring within 2–3 hours. Distribution into human body tissues and fluids not fully characterized. In animals, the drug is distributed mainly into the liver, with lower concentrations being distributed into the brain, lungs, kidneys, spleen, and heart. Distributed into milk.
Plasma Protein Binding: About 92%.
Exact metabolic fate not clearly established, but appears to be principally metabolized in the liver by oxidative N-dealkylation of the piperidine nitrogen to form fluorophenylcarbonic acids and piperidine metabolites (which appear to be inactive), and by reduction of the butyrophenone carbonyl to the carbinol, forming hydroxyhaloperidol.
Limited data suggest that the reduced metabolite, hydroxyhaloperidol, has some pharmacologic activity, although its activity appears to be less than that of haloperidol.
Butyrophenones
[view] =>Butyrophenones
) ) [field_precautions] => Array ( [0] => Array ( [value] => Possible risk factors for leukopenia/neutropenia include pre-existing low white blood cell count (WBC) and history of drug-induced leukopenia/neutropenia. Patients with a history of a clinically significant low WBC or a drug-induced leukopenia/neutropenia should have their complete blood count (CBC) monitored frequently during the first few months of therapy and discontinuation of Haloperidol should be considered at the first sign of a clinically significant decline in WBC in the absence of other causative factors. Patients: • with clinically significant neutropenia should be carefully monitored for fever or other symptoms or signs of infection and treated promptly if such symptoms or signs occur. Patients with severe neutropenia (absolute neutrophil count < 1000/mm3) should discontinue Haloperidol and have their WBC followed until recovery. • with severe cardiovascular disorders, because of the possibility of transient hypotension and/or precipitation of anginal pain. Should hypotension occur and a vasopressor be required, epinephrine should not be used since Haloperidol may block its vasopressor activity and paradoxical further lowering of the blood pressure may occur. Instead, metaraminol, phenylephrine or norepinephrine should be used. • receiving anticonvulsant medications, with a history of seizures, or with EEG abnormalities, because Haloperidol may lower the convulsive threshold. If indicated, adequate anticonvulsant therapy should be concomitantly maintained. • with known allergies, or with a history of allergic reactions to drugs. • receiving anticoagulants, since an isolated instance of interference occurred with the effects of one anticoagulant (phenindione). [format] => 1 [safe] =>Possible risk factors for leukopenia/neutropenia include pre-existing low white blood cell count (WBC) and history of drug-induced leukopenia/neutropenia. Patients with a history of a clinically significant low WBC or a drug-induced leukopenia/neutropenia should have their complete blood count (CBC) monitored frequently during the first few months of therapy and discontinuation of Haloperidol should be considered at the first sign of a clinically significant decline in WBC in the absence of other causative factors.
Patients:
• with clinically significant neutropenia should be carefully monitored for fever or other symptoms or signs of infection and treated promptly if such symptoms or signs occur. Patients with severe neutropenia (absolute neutrophil count < 1000/mm3) should discontinue Haloperidol and have their WBC followed until recovery.
• with severe cardiovascular disorders, because of the possibility of transient hypotension and/or precipitation of anginal pain. Should hypotension occur and a vasopressor be required, epinephrine should not be used since Haloperidol may block its vasopressor activity and paradoxical further lowering of the blood pressure may occur. Instead, metaraminol, phenylephrine or norepinephrine should be used.
• receiving anticonvulsant medications, with a history of seizures, or with EEG abnormalities, because Haloperidol may lower the convulsive threshold. If indicated, adequate anticonvulsant therapy should be concomitantly maintained.
• with known allergies, or with a history of allergic reactions to drugs.
• receiving anticoagulants, since an isolated instance of interference occurred with the effects of one anticoagulant (phenindione).
Possible risk factors for leukopenia/neutropenia include pre-existing low white blood cell count (WBC) and history of drug-induced leukopenia/neutropenia. Patients with a history of a clinically significant low WBC or a drug-induced leukopenia/neutropenia should have their complete blood count (CBC) monitored frequently during the first few months of therapy and discontinuation of Haloperidol should be considered at the first sign of a clinically significant decline in WBC in the absence of other causative factors.
Patients:
• with clinically significant neutropenia should be carefully monitored for fever or other symptoms or signs of infection and treated promptly if such symptoms or signs occur. Patients with severe neutropenia (absolute neutrophil count < 1000/mm3) should discontinue Haloperidol and have their WBC followed until recovery.
• with severe cardiovascular disorders, because of the possibility of transient hypotension and/or precipitation of anginal pain. Should hypotension occur and a vasopressor be required, epinephrine should not be used since Haloperidol may block its vasopressor activity and paradoxical further lowering of the blood pressure may occur. Instead, metaraminol, phenylephrine or norepinephrine should be used.
• receiving anticonvulsant medications, with a history of seizures, or with EEG abnormalities, because Haloperidol may lower the convulsive threshold. If indicated, adequate anticonvulsant therapy should be concomitantly maintained.
• with known allergies, or with a history of allergic reactions to drugs.
• receiving anticoagulants, since an isolated instance of interference occurred with the effects of one anticoagulant (phenindione).
category C
[view] =>category C
) ) [field_references] => Array ( [0] => Array ( [value] => [format] => [safe] => [view] => ) ) [field_side_effects] => Array ( [0] => Array ( [value] => • dizziness, fainting, fast or pounding heartbeat; • restless muscle movements in your eyes, tongue, jaw, or neck; • tremor (uncontrolled shaking); • seizure (convulsions); • pale skin, easy bruising or bleeding, flu symptoms; • very stiff (rigid) muscles, high fever, sweating, confusion, fast or uneven heartbeats, tremors, feeling like you might pass out; • stabbing chest pain, feeling short of breath, cough with yellow or green mucus; • sudden mood changes, agitation, hallucinations, unusual thoughts or behavior; or • jaundice (yellowing of your skin or eyes). Less serious side effects may include: • headache, dizziness, spinning sensation, drowsiness; • sleep problems (insomnia); • feeling restless or anxious; • mild skin rash or itching; • breast enlargement, irregular menstrual periods, loss of interest in sex; or • dry mouth, blurred vision, urinating less than usual. [format] => 1 [safe] =>• dizziness, fainting, fast or pounding heartbeat;
• restless muscle movements in your eyes, tongue, jaw, or neck;
• tremor (uncontrolled shaking);
• seizure (convulsions);
• pale skin, easy bruising or bleeding, flu symptoms;
• very stiff (rigid) muscles, high fever, sweating, confusion, fast or uneven heartbeats, tremors, feeling like you might pass out;
• stabbing chest pain, feeling short of breath, cough with yellow or green mucus;
• sudden mood changes, agitation, hallucinations, unusual thoughts or behavior; or
• jaundice (yellowing of your skin or eyes).
Less serious side effects may include:
• headache, dizziness, spinning sensation, drowsiness;
• sleep problems (insomnia);
• feeling restless or anxious;
• mild skin rash or itching;
• breast enlargement, irregular menstrual periods, loss of interest in sex; or
• dry mouth, blurred vision, urinating less than usual.
• dizziness, fainting, fast or pounding heartbeat;
• restless muscle movements in your eyes, tongue, jaw, or neck;
• tremor (uncontrolled shaking);
• seizure (convulsions);
• pale skin, easy bruising or bleeding, flu symptoms;
• very stiff (rigid) muscles, high fever, sweating, confusion, fast or uneven heartbeats, tremors, feeling like you might pass out;
• stabbing chest pain, feeling short of breath, cough with yellow or green mucus;
• sudden mood changes, agitation, hallucinations, unusual thoughts or behavior; or
• jaundice (yellowing of your skin or eyes).
Less serious side effects may include:
• headache, dizziness, spinning sensation, drowsiness;
• sleep problems (insomnia);
• feeling restless or anxious;
• mild skin rash or itching;
• breast enlargement, irregular menstrual periods, loss of interest in sex; or
• dry mouth, blurred vision, urinating less than usual.
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
Antipsychotic
[view] =>Antipsychotic
) ) [field_related_products] => Array ( [0] => Array ( [nid] => [i18nsync] => 1 [safe] => Array ( ) [view] => ) [1] => Array ( [nid] => [i18nsync] => 1 [safe] => Array ( ) [view] => ) [2] => Array ( [nid] => [i18nsync] => 1 [safe] => Array ( ) [view] => ) ) [taxonomy] => Array ( [4] => stdClass Object ( [tid] => 4 [vid] => 1 [name] => Antiparkinson Drugs, Antidepressants,Antiepileptics, Anxiolytic Sedative, Hypnotics and Antipsychotics [description] => [weight] => 2 [language] => [trid] => 0 [v_weight_unused] => 0 ) ) [build_mode] => 0 [readmore] => 1 [content] => Array ( [field_one_image] => Array ( [#type_name] => product [#context] => full [#field_name] => field_one_image [#post_render] => Array ( [0] => content_field_wrapper_post_render ) [#weight] => -3 [field] => Array ( [#description] => [items] => Array ( [0] => Array ( [#formatter] => image_plain [#node] => stdClass Object *RECURSION* [#type_name] => product [#field_name] => field_one_image [#weight] => 0 [#theme] => imagefield_formatter_image_plain [#item] => Array ( [fid] => 184 [uid] => 1 [filename] => haloperidol_s.jpg [filepath] => sites/default/files/images/haloperidol_s.jpg [filemime] => image/jpeg [filesize] => 51261 [status] => 1 [timestamp] => 1329489015 [list] => 1 [data] => Array ( [alt] => [title] => ) [i18nsync] => 1 [nid] => 272 [#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] => )
[#title] =>
[#description] =>
[#children] =>
)
[#title] =>
[#description] =>
[#children] =>  [#printed] => 1
)
[#single] => 1
[#attributes] => Array
(
)
[#required] =>
[#parents] => Array
(
)
[#tree] =>
[#context] => full
[#page] => 1
[#field_name] => field_one_image
[#title] => Image
[#access] => 1
[#label_display] => above
[#teaser] =>
[#node] => stdClass Object
*RECURSION*
[#type] => content_field
[#children] =>
[#printed] => 1
)
[#single] => 1
[#attributes] => Array
(
)
[#required] =>
[#parents] => Array
(
)
[#tree] =>
[#context] => full
[#page] => 1
[#field_name] => field_one_image
[#title] => Image
[#access] => 1
[#label_display] => above
[#teaser] =>
[#node] => stdClass Object
*RECURSION*
[#type] => content_field
[#children] =>  [#printed] => 1
)
[#title] =>
[#description] =>
[#children] =>
[#printed] => 1
)
[#title] =>
[#description] =>
[#children] => 
HALODIC®
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>HALODIC®
) [#title] => [#description] => [#children] =>HALODIC®
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_brand_name [#title] => Brand Name [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>HALODIC®
[#printed] => 1 ) [#title] => [#description] => [#children] =>HALODIC®
Injection 5mg/1ml
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Injection 5mg/1ml
) [#title] => [#description] => [#children] =>Injection 5mg/1ml
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_dosage_form [#title] => Dosage Form [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Injection 5mg/1ml
[#printed] => 1 ) [#title] => [#description] => [#children] =>Injection 5mg/1ml
Butyrophenones
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Butyrophenones
) [#title] => [#description] => [#children] =>Butyrophenones
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_pharmacological_category [#title] => Pharmacological Category [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Butyrophenones
[#printed] => 1 ) [#title] => [#description] => [#children] =>Butyrophenones
Antipsychotic
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Antipsychotic
) [#title] => [#description] => [#children] =>Antipsychotic
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_therapeutic_category [#title] => Therapeutic Category [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Antipsychotic
[#printed] => 1 ) [#title] => [#description] => [#children] =>Antipsychotic
category C
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>category C
) [#title] => [#description] => [#children] =>category C
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_pregnancy_category [#title] => Pregnancy Category [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>category C
[#printed] => 1 ) [#title] => [#description] => [#children] =>category C
Precise mechanism of antipsychotic action is unclear, but appears to depress the CNS at the subcortical level of the brain, midbrain, and brain stem reticular formation; appears to inhibit the ascending reticular activating system of the brain stem (possibly through the caudate nucleus), thereby interrupting the impulse between the diencephalon and the cortex.
May antagonize actions of glutamic acid within the extrapyramidal system. Inhibition of catecholamine receptors may also be important in the mode of action; may also inhibit the reuptake of various neurotransmitters in the midbrain.
[#title] => [#description] => [#printed] => 1 ) [field_pharmacokinetics] => Array ( [#type_name] => product [#context] => full [#field_name] => field_pharmacokinetics [#post_render] => Array ( [0] => content_field_wrapper_post_render ) [#weight] => 4 [field] => Array ( [#description] => [items] => Array ( [0] => Array ( [#formatter] => default [#node] => stdClass Object *RECURSION* [#type_name] => product [#field_name] => field_pharmacokinetics [#weight] => 0 [#theme] => text_formatter_default [#item] => Array ( [value] => Following IM administration of haloperidol lactate, peak plasma haloperidol concentrations occur within 10–20 minutes. Following IM administration of haloperidol lactate, peak pharmacologic action occurs within 30–45 minutes; in acutely agitated patients, control of psychotic manifestations may become apparent within 30–60 minutes, with substantial improvement often occurring within 2–3 hours. Distribution into human body tissues and fluids not fully characterized. In animals, the drug is distributed mainly into the liver, with lower concentrations being distributed into the brain, lungs, kidneys, spleen, and heart. Distributed into milk. Plasma Protein Binding: About 92%. Exact metabolic fate not clearly established, but appears to be principally metabolized in the liver by oxidative N-dealkylation of the piperidine nitrogen to form fluorophenylcarbonic acids and piperidine metabolites (which appear to be inactive), and by reduction of the butyrophenone carbonyl to the carbinol, forming hydroxyhaloperidol. Limited data suggest that the reduced metabolite, hydroxyhaloperidol, has some pharmacologic activity, although its activity appears to be less than that of haloperidol. [format] => 1 [safe] =>Following IM administration of haloperidol lactate, peak plasma haloperidol concentrations occur within 10–20 minutes. Following IM administration of haloperidol lactate, peak pharmacologic action occurs within 30–45 minutes; in acutely agitated patients, control of psychotic manifestations may become apparent within 30–60 minutes, with substantial improvement often occurring within 2–3 hours. Distribution into human body tissues and fluids not fully characterized. In animals, the drug is distributed mainly into the liver, with lower concentrations being distributed into the brain, lungs, kidneys, spleen, and heart. Distributed into milk.
Plasma Protein Binding: About 92%.
Exact metabolic fate not clearly established, but appears to be principally metabolized in the liver by oxidative N-dealkylation of the piperidine nitrogen to form fluorophenylcarbonic acids and piperidine metabolites (which appear to be inactive), and by reduction of the butyrophenone carbonyl to the carbinol, forming hydroxyhaloperidol.
Limited data suggest that the reduced metabolite, hydroxyhaloperidol, has some pharmacologic activity, although its activity appears to be less than that of haloperidol.
Following IM administration of haloperidol lactate, peak plasma haloperidol concentrations occur within 10–20 minutes. Following IM administration of haloperidol lactate, peak pharmacologic action occurs within 30–45 minutes; in acutely agitated patients, control of psychotic manifestations may become apparent within 30–60 minutes, with substantial improvement often occurring within 2–3 hours. Distribution into human body tissues and fluids not fully characterized. In animals, the drug is distributed mainly into the liver, with lower concentrations being distributed into the brain, lungs, kidneys, spleen, and heart. Distributed into milk.
Plasma Protein Binding: About 92%.
Exact metabolic fate not clearly established, but appears to be principally metabolized in the liver by oxidative N-dealkylation of the piperidine nitrogen to form fluorophenylcarbonic acids and piperidine metabolites (which appear to be inactive), and by reduction of the butyrophenone carbonyl to the carbinol, forming hydroxyhaloperidol.
Limited data suggest that the reduced metabolite, hydroxyhaloperidol, has some pharmacologic activity, although its activity appears to be less than that of haloperidol.
Following IM administration of haloperidol lactate, peak plasma haloperidol concentrations occur within 10–20 minutes. Following IM administration of haloperidol lactate, peak pharmacologic action occurs within 30–45 minutes; in acutely agitated patients, control of psychotic manifestations may become apparent within 30–60 minutes, with substantial improvement often occurring within 2–3 hours. Distribution into human body tissues and fluids not fully characterized. In animals, the drug is distributed mainly into the liver, with lower concentrations being distributed into the brain, lungs, kidneys, spleen, and heart. Distributed into milk.
Plasma Protein Binding: About 92%.
Exact metabolic fate not clearly established, but appears to be principally metabolized in the liver by oxidative N-dealkylation of the piperidine nitrogen to form fluorophenylcarbonic acids and piperidine metabolites (which appear to be inactive), and by reduction of the butyrophenone carbonyl to the carbinol, forming hydroxyhaloperidol.
Limited data suggest that the reduced metabolite, hydroxyhaloperidol, has some pharmacologic activity, although its activity appears to be less than that of haloperidol.
Following IM administration of haloperidol lactate, peak plasma haloperidol concentrations occur within 10–20 minutes. Following IM administration of haloperidol lactate, peak pharmacologic action occurs within 30–45 minutes; in acutely agitated patients, control of psychotic manifestations may become apparent within 30–60 minutes, with substantial improvement often occurring within 2–3 hours. Distribution into human body tissues and fluids not fully characterized. In animals, the drug is distributed mainly into the liver, with lower concentrations being distributed into the brain, lungs, kidneys, spleen, and heart. Distributed into milk.
Plasma Protein Binding: About 92%.
Exact metabolic fate not clearly established, but appears to be principally metabolized in the liver by oxidative N-dealkylation of the piperidine nitrogen to form fluorophenylcarbonic acids and piperidine metabolites (which appear to be inactive), and by reduction of the butyrophenone carbonyl to the carbinol, forming hydroxyhaloperidol.
Limited data suggest that the reduced metabolite, hydroxyhaloperidol, has some pharmacologic activity, although its activity appears to be less than that of haloperidol.
Following IM administration of haloperidol lactate, peak plasma haloperidol concentrations occur within 10–20 minutes. Following IM administration of haloperidol lactate, peak pharmacologic action occurs within 30–45 minutes; in acutely agitated patients, control of psychotic manifestations may become apparent within 30–60 minutes, with substantial improvement often occurring within 2–3 hours. Distribution into human body tissues and fluids not fully characterized. In animals, the drug is distributed mainly into the liver, with lower concentrations being distributed into the brain, lungs, kidneys, spleen, and heart. Distributed into milk.
Plasma Protein Binding: About 92%.
Exact metabolic fate not clearly established, but appears to be principally metabolized in the liver by oxidative N-dealkylation of the piperidine nitrogen to form fluorophenylcarbonic acids and piperidine metabolites (which appear to be inactive), and by reduction of the butyrophenone carbonyl to the carbinol, forming hydroxyhaloperidol.
Limited data suggest that the reduced metabolite, hydroxyhaloperidol, has some pharmacologic activity, although its activity appears to be less than that of haloperidol.
Haloperidol is used to treat schizophrenia. It is also used to control motor and speech tics in people with Tourette's syndrome.
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>Haloperidol is used to treat schizophrenia. It is also used to control motor and speech tics in people with Tourette's syndrome.
) [#title] => [#description] => [#children] =>Haloperidol is used to treat schizophrenia. It is also used to control motor and speech tics in people with Tourette's syndrome.
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_indications [#title] => Indications [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>Haloperidol is used to treat schizophrenia. It is also used to control motor and speech tics in people with Tourette's syndrome.
[#printed] => 1 ) [#title] => [#description] => [#children] =>Haloperidol is used to treat schizophrenia. It is also used to control motor and speech tics in people with Tourette's syndrome.
• Severe toxic CNS depression or comatose states from any cause.
• Parkinsonian syndrome.
• Hypersensitivity to haloperidol.
• Severe toxic CNS depression or comatose states from any cause.
• Parkinsonian syndrome.
• Hypersensitivity to haloperidol.
• Severe toxic CNS depression or comatose states from any cause.
• Parkinsonian syndrome.
• Hypersensitivity to haloperidol.
• Severe toxic CNS depression or comatose states from any cause.
• Parkinsonian syndrome.
• Hypersensitivity to haloperidol.
• Severe toxic CNS depression or comatose states from any cause.
• Parkinsonian syndrome.
• Hypersensitivity to haloperidol.
Possible risk factors for leukopenia/neutropenia include pre-existing low white blood cell count (WBC) and history of drug-induced leukopenia/neutropenia. Patients with a history of a clinically significant low WBC or a drug-induced leukopenia/neutropenia should have their complete blood count (CBC) monitored frequently during the first few months of therapy and discontinuation of Haloperidol should be considered at the first sign of a clinically significant decline in WBC in the absence of other causative factors.
Patients:
• with clinically significant neutropenia should be carefully monitored for fever or other symptoms or signs of infection and treated promptly if such symptoms or signs occur. Patients with severe neutropenia (absolute neutrophil count < 1000/mm3) should discontinue Haloperidol and have their WBC followed until recovery.
• with severe cardiovascular disorders, because of the possibility of transient hypotension and/or precipitation of anginal pain. Should hypotension occur and a vasopressor be required, epinephrine should not be used since Haloperidol may block its vasopressor activity and paradoxical further lowering of the blood pressure may occur. Instead, metaraminol, phenylephrine or norepinephrine should be used.
• receiving anticonvulsant medications, with a history of seizures, or with EEG abnormalities, because Haloperidol may lower the convulsive threshold. If indicated, adequate anticonvulsant therapy should be concomitantly maintained.
• with known allergies, or with a history of allergic reactions to drugs.
• receiving anticoagulants, since an isolated instance of interference occurred with the effects of one anticoagulant (phenindione).
Possible risk factors for leukopenia/neutropenia include pre-existing low white blood cell count (WBC) and history of drug-induced leukopenia/neutropenia. Patients with a history of a clinically significant low WBC or a drug-induced leukopenia/neutropenia should have their complete blood count (CBC) monitored frequently during the first few months of therapy and discontinuation of Haloperidol should be considered at the first sign of a clinically significant decline in WBC in the absence of other causative factors.
Patients:
• with clinically significant neutropenia should be carefully monitored for fever or other symptoms or signs of infection and treated promptly if such symptoms or signs occur. Patients with severe neutropenia (absolute neutrophil count < 1000/mm3) should discontinue Haloperidol and have their WBC followed until recovery.
• with severe cardiovascular disorders, because of the possibility of transient hypotension and/or precipitation of anginal pain. Should hypotension occur and a vasopressor be required, epinephrine should not be used since Haloperidol may block its vasopressor activity and paradoxical further lowering of the blood pressure may occur. Instead, metaraminol, phenylephrine or norepinephrine should be used.
• receiving anticonvulsant medications, with a history of seizures, or with EEG abnormalities, because Haloperidol may lower the convulsive threshold. If indicated, adequate anticonvulsant therapy should be concomitantly maintained.
• with known allergies, or with a history of allergic reactions to drugs.
• receiving anticoagulants, since an isolated instance of interference occurred with the effects of one anticoagulant (phenindione).
Possible risk factors for leukopenia/neutropenia include pre-existing low white blood cell count (WBC) and history of drug-induced leukopenia/neutropenia. Patients with a history of a clinically significant low WBC or a drug-induced leukopenia/neutropenia should have their complete blood count (CBC) monitored frequently during the first few months of therapy and discontinuation of Haloperidol should be considered at the first sign of a clinically significant decline in WBC in the absence of other causative factors.
Patients:
• with clinically significant neutropenia should be carefully monitored for fever or other symptoms or signs of infection and treated promptly if such symptoms or signs occur. Patients with severe neutropenia (absolute neutrophil count < 1000/mm3) should discontinue Haloperidol and have their WBC followed until recovery.
• with severe cardiovascular disorders, because of the possibility of transient hypotension and/or precipitation of anginal pain. Should hypotension occur and a vasopressor be required, epinephrine should not be used since Haloperidol may block its vasopressor activity and paradoxical further lowering of the blood pressure may occur. Instead, metaraminol, phenylephrine or norepinephrine should be used.
• receiving anticonvulsant medications, with a history of seizures, or with EEG abnormalities, because Haloperidol may lower the convulsive threshold. If indicated, adequate anticonvulsant therapy should be concomitantly maintained.
• with known allergies, or with a history of allergic reactions to drugs.
• receiving anticoagulants, since an isolated instance of interference occurred with the effects of one anticoagulant (phenindione).
Possible risk factors for leukopenia/neutropenia include pre-existing low white blood cell count (WBC) and history of drug-induced leukopenia/neutropenia. Patients with a history of a clinically significant low WBC or a drug-induced leukopenia/neutropenia should have their complete blood count (CBC) monitored frequently during the first few months of therapy and discontinuation of Haloperidol should be considered at the first sign of a clinically significant decline in WBC in the absence of other causative factors.
Patients:
• with clinically significant neutropenia should be carefully monitored for fever or other symptoms or signs of infection and treated promptly if such symptoms or signs occur. Patients with severe neutropenia (absolute neutrophil count < 1000/mm3) should discontinue Haloperidol and have their WBC followed until recovery.
• with severe cardiovascular disorders, because of the possibility of transient hypotension and/or precipitation of anginal pain. Should hypotension occur and a vasopressor be required, epinephrine should not be used since Haloperidol may block its vasopressor activity and paradoxical further lowering of the blood pressure may occur. Instead, metaraminol, phenylephrine or norepinephrine should be used.
• receiving anticonvulsant medications, with a history of seizures, or with EEG abnormalities, because Haloperidol may lower the convulsive threshold. If indicated, adequate anticonvulsant therapy should be concomitantly maintained.
• with known allergies, or with a history of allergic reactions to drugs.
• receiving anticoagulants, since an isolated instance of interference occurred with the effects of one anticoagulant (phenindione).
Possible risk factors for leukopenia/neutropenia include pre-existing low white blood cell count (WBC) and history of drug-induced leukopenia/neutropenia. Patients with a history of a clinically significant low WBC or a drug-induced leukopenia/neutropenia should have their complete blood count (CBC) monitored frequently during the first few months of therapy and discontinuation of Haloperidol should be considered at the first sign of a clinically significant decline in WBC in the absence of other causative factors.
Patients:
• with clinically significant neutropenia should be carefully monitored for fever or other symptoms or signs of infection and treated promptly if such symptoms or signs occur. Patients with severe neutropenia (absolute neutrophil count < 1000/mm3) should discontinue Haloperidol and have their WBC followed until recovery.
• with severe cardiovascular disorders, because of the possibility of transient hypotension and/or precipitation of anginal pain. Should hypotension occur and a vasopressor be required, epinephrine should not be used since Haloperidol may block its vasopressor activity and paradoxical further lowering of the blood pressure may occur. Instead, metaraminol, phenylephrine or norepinephrine should be used.
• receiving anticonvulsant medications, with a history of seizures, or with EEG abnormalities, because Haloperidol may lower the convulsive threshold. If indicated, adequate anticonvulsant therapy should be concomitantly maintained.
• with known allergies, or with a history of allergic reactions to drugs.
• receiving anticoagulants, since an isolated instance of interference occurred with the effects of one anticoagulant (phenindione).
• arsenic trioxide (Trisenox)
• a blood thinner such as warfarin (Coumadin)
• lithium
• seizure medication
• rifampin
• tacrolimus (Prograf)
• an antibiotic such as clarithromycin (Biaxin), erythromycin ,levofloxacin (Levaquin), moxifloxacin (Avelox), or pentamidine
• an antidepressant such as amitriptylline (Elavil), clomipramine (Anafranil), or desipramine
• anti-malaria medications such as chloroquine or mefloquine
• heart rhythm medicine such as amiodarone (Cordarone), dofetilide, disopyramide, dronedarone, ibutilide, procainamide, propafenone, quinidine, or sotalol
• medicine to prevent or treat nausea and vomiting such as dolasetron (Anzemet), droperidol or ondansetron (Zofran);
• medicines to treat psychiatric disorders, such as chlorpromazine, clozapine, pimozide (Orap), thioridazine (Mellaril), or ziprasidone
• migraine headache medicine such as sumatriptan or zolmitriptan (Zomig); or
• narcotic medication such as methadone
• arsenic trioxide (Trisenox)
• a blood thinner such as warfarin (Coumadin)
• lithium
• seizure medication
• rifampin
• tacrolimus (Prograf)
• an antibiotic such as clarithromycin (Biaxin), erythromycin ,levofloxacin (Levaquin), moxifloxacin (Avelox), or pentamidine
• an antidepressant such as amitriptylline (Elavil), clomipramine (Anafranil), or desipramine
• anti-malaria medications such as chloroquine or mefloquine
• heart rhythm medicine such as amiodarone (Cordarone), dofetilide, disopyramide, dronedarone, ibutilide, procainamide, propafenone, quinidine, or sotalol
• medicine to prevent or treat nausea and vomiting such as dolasetron (Anzemet), droperidol or ondansetron (Zofran);
• medicines to treat psychiatric disorders, such as chlorpromazine, clozapine, pimozide (Orap), thioridazine (Mellaril), or ziprasidone
• migraine headache medicine such as sumatriptan or zolmitriptan (Zomig); or
• narcotic medication such as methadone
• arsenic trioxide (Trisenox)
• a blood thinner such as warfarin (Coumadin)
• lithium
• seizure medication
• rifampin
• tacrolimus (Prograf)
• an antibiotic such as clarithromycin (Biaxin), erythromycin ,levofloxacin (Levaquin), moxifloxacin (Avelox), or pentamidine
• an antidepressant such as amitriptylline (Elavil), clomipramine (Anafranil), or desipramine
• anti-malaria medications such as chloroquine or mefloquine
• heart rhythm medicine such as amiodarone (Cordarone), dofetilide, disopyramide, dronedarone, ibutilide, procainamide, propafenone, quinidine, or sotalol
• medicine to prevent or treat nausea and vomiting such as dolasetron (Anzemet), droperidol or ondansetron (Zofran);
• medicines to treat psychiatric disorders, such as chlorpromazine, clozapine, pimozide (Orap), thioridazine (Mellaril), or ziprasidone
• migraine headache medicine such as sumatriptan or zolmitriptan (Zomig); or
• narcotic medication such as methadone
• arsenic trioxide (Trisenox)
• a blood thinner such as warfarin (Coumadin)
• lithium
• seizure medication
• rifampin
• tacrolimus (Prograf)
• an antibiotic such as clarithromycin (Biaxin), erythromycin ,levofloxacin (Levaquin), moxifloxacin (Avelox), or pentamidine
• an antidepressant such as amitriptylline (Elavil), clomipramine (Anafranil), or desipramine
• anti-malaria medications such as chloroquine or mefloquine
• heart rhythm medicine such as amiodarone (Cordarone), dofetilide, disopyramide, dronedarone, ibutilide, procainamide, propafenone, quinidine, or sotalol
• medicine to prevent or treat nausea and vomiting such as dolasetron (Anzemet), droperidol or ondansetron (Zofran);
• medicines to treat psychiatric disorders, such as chlorpromazine, clozapine, pimozide (Orap), thioridazine (Mellaril), or ziprasidone
• migraine headache medicine such as sumatriptan or zolmitriptan (Zomig); or
• narcotic medication such as methadone
• arsenic trioxide (Trisenox)
• a blood thinner such as warfarin (Coumadin)
• lithium
• seizure medication
• rifampin
• tacrolimus (Prograf)
• an antibiotic such as clarithromycin (Biaxin), erythromycin ,levofloxacin (Levaquin), moxifloxacin (Avelox), or pentamidine
• an antidepressant such as amitriptylline (Elavil), clomipramine (Anafranil), or desipramine
• anti-malaria medications such as chloroquine or mefloquine
• heart rhythm medicine such as amiodarone (Cordarone), dofetilide, disopyramide, dronedarone, ibutilide, procainamide, propafenone, quinidine, or sotalol
• medicine to prevent or treat nausea and vomiting such as dolasetron (Anzemet), droperidol or ondansetron (Zofran);
• medicines to treat psychiatric disorders, such as chlorpromazine, clozapine, pimozide (Orap), thioridazine (Mellaril), or ziprasidone
• migraine headache medicine such as sumatriptan or zolmitriptan (Zomig); or
• narcotic medication such as methadone
• dizziness, fainting, fast or pounding heartbeat;
• restless muscle movements in your eyes, tongue, jaw, or neck;
• tremor (uncontrolled shaking);
• seizure (convulsions);
• pale skin, easy bruising or bleeding, flu symptoms;
• very stiff (rigid) muscles, high fever, sweating, confusion, fast or uneven heartbeats, tremors, feeling like you might pass out;
• stabbing chest pain, feeling short of breath, cough with yellow or green mucus;
• sudden mood changes, agitation, hallucinations, unusual thoughts or behavior; or
• jaundice (yellowing of your skin or eyes).
Less serious side effects may include:
• headache, dizziness, spinning sensation, drowsiness;
• sleep problems (insomnia);
• feeling restless or anxious;
• mild skin rash or itching;
• breast enlargement, irregular menstrual periods, loss of interest in sex; or
• dry mouth, blurred vision, urinating less than usual.
• dizziness, fainting, fast or pounding heartbeat;
• restless muscle movements in your eyes, tongue, jaw, or neck;
• tremor (uncontrolled shaking);
• seizure (convulsions);
• pale skin, easy bruising or bleeding, flu symptoms;
• very stiff (rigid) muscles, high fever, sweating, confusion, fast or uneven heartbeats, tremors, feeling like you might pass out;
• stabbing chest pain, feeling short of breath, cough with yellow or green mucus;
• sudden mood changes, agitation, hallucinations, unusual thoughts or behavior; or
• jaundice (yellowing of your skin or eyes).
Less serious side effects may include:
• headache, dizziness, spinning sensation, drowsiness;
• sleep problems (insomnia);
• feeling restless or anxious;
• mild skin rash or itching;
• breast enlargement, irregular menstrual periods, loss of interest in sex; or
• dry mouth, blurred vision, urinating less than usual.
• dizziness, fainting, fast or pounding heartbeat;
• restless muscle movements in your eyes, tongue, jaw, or neck;
• tremor (uncontrolled shaking);
• seizure (convulsions);
• pale skin, easy bruising or bleeding, flu symptoms;
• very stiff (rigid) muscles, high fever, sweating, confusion, fast or uneven heartbeats, tremors, feeling like you might pass out;
• stabbing chest pain, feeling short of breath, cough with yellow or green mucus;
• sudden mood changes, agitation, hallucinations, unusual thoughts or behavior; or
• jaundice (yellowing of your skin or eyes).
Less serious side effects may include:
• headache, dizziness, spinning sensation, drowsiness;
• sleep problems (insomnia);
• feeling restless or anxious;
• mild skin rash or itching;
• breast enlargement, irregular menstrual periods, loss of interest in sex; or
• dry mouth, blurred vision, urinating less than usual.
• dizziness, fainting, fast or pounding heartbeat;
• restless muscle movements in your eyes, tongue, jaw, or neck;
• tremor (uncontrolled shaking);
• seizure (convulsions);
• pale skin, easy bruising or bleeding, flu symptoms;
• very stiff (rigid) muscles, high fever, sweating, confusion, fast or uneven heartbeats, tremors, feeling like you might pass out;
• stabbing chest pain, feeling short of breath, cough with yellow or green mucus;
• sudden mood changes, agitation, hallucinations, unusual thoughts or behavior; or
• jaundice (yellowing of your skin or eyes).
Less serious side effects may include:
• headache, dizziness, spinning sensation, drowsiness;
• sleep problems (insomnia);
• feeling restless or anxious;
• mild skin rash or itching;
• breast enlargement, irregular menstrual periods, loss of interest in sex; or
• dry mouth, blurred vision, urinating less than usual.
• dizziness, fainting, fast or pounding heartbeat;
• restless muscle movements in your eyes, tongue, jaw, or neck;
• tremor (uncontrolled shaking);
• seizure (convulsions);
• pale skin, easy bruising or bleeding, flu symptoms;
• very stiff (rigid) muscles, high fever, sweating, confusion, fast or uneven heartbeats, tremors, feeling like you might pass out;
• stabbing chest pain, feeling short of breath, cough with yellow or green mucus;
• sudden mood changes, agitation, hallucinations, unusual thoughts or behavior; or
• jaundice (yellowing of your skin or eyes).
Less serious side effects may include:
• headache, dizziness, spinning sensation, drowsiness;
• sleep problems (insomnia);
• feeling restless or anxious;
• mild skin rash or itching;
• breast enlargement, irregular menstrual periods, loss of interest in sex; or
• dry mouth, blurred vision, urinating less than usual.
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
• Store below 30 C°
• Protect from light and freezing
• Injection 5mg/1ml: Box of 5 Ampoules
[#delta] => 0 ) [#title] => [#description] => [#theme_used] => 1 [#printed] => 1 [#type] => [#value] => [#prefix] => [#suffix] => [#children] =>• Injection 5mg/1ml: Box of 5 Ampoules
) [#title] => [#description] => [#children] =>• Injection 5mg/1ml: Box of 5 Ampoules
[#printed] => 1 ) [#single] => 1 [#attributes] => Array ( ) [#required] => [#parents] => Array ( ) [#tree] => [#context] => full [#page] => 1 [#field_name] => field_packing [#title] => Packing [#access] => 1 [#label_display] => above [#teaser] => [#node] => stdClass Object *RECURSION* [#type] => content_field [#children] =>• Injection 5mg/1ml: Box of 5 Ampoules
[#printed] => 1 ) [#title] => [#description] => [#children] =>• Injection 5mg/1ml: Box of 5 Ampoules
HALODIC®
Injection 5mg/1ml
Butyrophenones
Antipsychotic
category C
Precise mechanism of antipsychotic action is unclear, but appears to depress the CNS at the subcortical level of the brain, midbrain, and brain stem reticular formation; appears to inhibit the ascending reticular activating system of the brain stem (possibly through the caudate nucleus), thereby interrupting the impulse between the diencephalon and the cortex.
May antagonize actions of glutamic acid within the extrapyramidal system. Inhibition of catecholamine receptors may also be important in the mode of action; may also inhibit the reuptake of various neurotransmitters in the midbrain.
Following IM administration of haloperidol lactate, peak plasma haloperidol concentrations occur within 10–20 minutes. Following IM administration of haloperidol lactate, peak pharmacologic action occurs within 30–45 minutes; in acutely agitated patients, control of psychotic manifestations may become apparent within 30–60 minutes, with substantial improvement often occurring within 2–3 hours. Distribution into human body tissues and fluids not fully characterized. In animals, the drug is distributed mainly into the liver, with lower concentrations being distributed into the brain, lungs, kidneys, spleen, and heart. Distributed into milk.
Plasma Protein Binding: About 92%.
Exact metabolic fate not clearly established, but appears to be principally metabolized in the liver by oxidative N-dealkylation of the piperidine nitrogen to form fluorophenylcarbonic acids and piperidine metabolites (which appear to be inactive), and by reduction of the butyrophenone carbonyl to the carbinol, forming hydroxyhaloperidol.
Limited data suggest that the reduced metabolite, hydroxyhaloperidol, has some pharmacologic activity, although its activity appears to be less than that of haloperidol.
Haloperidol is used to treat schizophrenia. It is also used to control motor and speech tics in people with Tourette's syndrome.
• Severe toxic CNS depression or comatose states from any cause.
• Parkinsonian syndrome.
• Hypersensitivity to haloperidol.
Possible risk factors for leukopenia/neutropenia include pre-existing low white blood cell count (WBC) and history of drug-induced leukopenia/neutropenia. Patients with a history of a clinically significant low WBC or a drug-induced leukopenia/neutropenia should have their complete blood count (CBC) monitored frequently during the first few months of therapy and discontinuation of Haloperidol should be considered at the first sign of a clinically significant decline in WBC in the absence of other causative factors.
Patients:
• with clinically significant neutropenia should be carefully monitored for fever or other symptoms or signs of infection and treated promptly if such symptoms or signs occur. Patients with severe neutropenia (absolute neutrophil count < 1000/mm3) should discontinue Haloperidol and have their WBC followed until recovery.
• with severe cardiovascular disorders, because of the possibility of transient hypotension and/or precipitation of anginal pain. Should hypotension occur and a vasopressor be required, epinephrine should not be used since Haloperidol may block its vasopressor activity and paradoxical further lowering of the blood pressure may occur. Instead, metaraminol, phenylephrine or norepinephrine should be used.
• receiving anticonvulsant medications, with a history of seizures, or with EEG abnormalities, because Haloperidol may lower the convulsive threshold. If indicated, adequate anticonvulsant therapy should be concomitantly maintained.
• with known allergies, or with a history of allergic reactions to drugs.
• receiving anticoagulants, since an isolated instance of interference occurred with the effects of one anticoagulant (phenindione).
• arsenic trioxide (Trisenox)
• a blood thinner such as warfarin (Coumadin)
• lithium
• seizure medication
• rifampin
• tacrolimus (Prograf)
• an antibiotic such as clarithromycin (Biaxin), erythromycin ,levofloxacin (Levaquin), moxifloxacin (Avelox), or pentamidine
• an antidepressant such as amitriptylline (Elavil), clomipramine (Anafranil), or desipramine
• anti-malaria medications such as chloroquine or mefloquine
• heart rhythm medicine such as amiodarone (Cordarone), dofetilide, disopyramide, dronedarone, ibutilide, procainamide, propafenone, quinidine, or sotalol
• medicine to prevent or treat nausea and vomiting such as dolasetron (Anzemet), droperidol or ondansetron (Zofran);
• medicines to treat psychiatric disorders, such as chlorpromazine, clozapine, pimozide (Orap), thioridazine (Mellaril), or ziprasidone
• migraine headache medicine such as sumatriptan or zolmitriptan (Zomig); or
• narcotic medication such as methadone
• dizziness, fainting, fast or pounding heartbeat;
• restless muscle movements in your eyes, tongue, jaw, or neck;
• tremor (uncontrolled shaking);
• seizure (convulsions);
• pale skin, easy bruising or bleeding, flu symptoms;
• very stiff (rigid) muscles, high fever, sweating, confusion, fast or uneven heartbeats, tremors, feeling like you might pass out;
• stabbing chest pain, feeling short of breath, cough with yellow or green mucus;
• sudden mood changes, agitation, hallucinations, unusual thoughts or behavior; or
• jaundice (yellowing of your skin or eyes).
Less serious side effects may include:
• headache, dizziness, spinning sensation, drowsiness;
• sleep problems (insomnia);
• feeling restless or anxious;
• mild skin rash or itching;
• breast enlargement, irregular menstrual periods, loss of interest in sex; or
• dry mouth, blurred vision, urinating less than usual.
• Store below 30 C°
• Protect from light and freezing
• Injection 5mg/1ml: Box of 5 Ampoules